| ANAESTHESIA PEARLS |
| ET technology improves | ||||
| Cowan described how endotracheal tubes that were originally introduced in the 1970s often contributed to microaspiration. "Conventional endotracheal tubes have a barrel-shaped, high-volume, low-pressure cuff that provides an adequate air seal, but does not sufficiently seal the patient’s tracheal passageway from fluids. This means secretions from the mouth and digestive tract can potentially migrate through folds in the cuff into the patient’s lungs." | ||||
| Covidien’s TaperGuard line of endotracheal tubes gives intubated patients extra protection, she assured. "The tubes have a unique, taper-shaped cuff with a superior seal to help prevent secretions from entering the airways. The TaperGuard endotracheal tube has been shown to reduce microaspiration by an average of 90 percent compared to Mallinckrodt Hi-Lo endotracheal tubes.6 The TaperGuard Evac endotracheal tube combines the TaperGuard cuff with Mallinckrodt Evac technology, which enables continuous or intermittent drainage of secretions that collect above the cuff, providing additional protection against VAP(Ventilator Associated Pneumonia)"6 | ||||

| ||||
| Covidien TaperGuard | ||||
| New from Teleflex Medical, the Teleflex ISIS HVT is a convertible endotracheal tube that allows you to maintain current intubation procedures used for patients on short-term or long-term intubation. Teleflex ISIS HVT is supplied as components sold separately: an endotracheal tube with integrated suction port and a suction line. The suction port on the endotracheal tube allows for access to subglottic secretion removal when needed by attaching the separate suction line. This design improves access to subglottic suctioning, one of the clinical best practices for reducing early onset VAP. | ||||

| ||||
| Teleflex ISIS HVT convertible endotracheal tube | ||||
| With other subglottic secretion removal endotracheal tubes, the suction line is permanently attached and if the patient doesn’t get a subglottic secretion removal endotracheal tube at the time of initial intubation, the clinician needs to make the choice whether or not to extubate and reintubate the patient to provide the benefits of access to subglottic secretion removal. | ||||
| The Teleflex ISIS HVT endotracheal tube is priced slightly above the cost of a standard endotracheal tube to allow for wider usage and greater access to this practice. | ||||
| The suction line features an ergonomically designed suction connector for easy handling when connecting suction tubing and specially designed caps seal suction line when not in use. A pilot balloon in the endotracheal tube provides tactile feedback allowing for a visual gauge of cuff inflation. The High-Volume Taper (HVT) cuff is a thin-walled, high-volume, low-pressure, tapered cuff on the endotracheal tube which effectively seal at low pressures. A placement ring is included above the cuff on the endotracheal tube which provides a visual indication of when the tube has passed the vocal chords to aid in placement. Lastly, the dorsal suction lumen allows for the removal of accumulated secretions and its custom design reduces likelihood of mucus obstruction. | ||||
| To watch a video to learn more about the Teleflex ISIS HVT: click here | ||||
| The Kimberly-Clark KimVent Microcuff Endotracheal Tube is also designed to prevent the micro-aspiration of potentially infectious secretions into the lungs, thereby lowering the risk of VAP. The Microcuff ET’s unique cuff is made of an advanced microthin polyurethane material that allows the channels formed upon cuff inflation to ‘self-seal’ within the trachea, increasing protection against fluid leakage into the lungs. In addition, the KimVent Microcuff Endotracheal Tube has a longer length and cylindrical shape cuff, which provides better contact with the tracheal contour and increases protection against fluid leakage. | ||||
 Kimberly-Clark KimVent Microcuff |
The Kimberly-Clark KimVent Microcuff Endotracheal Tube is also designed to prevent the micro-aspiration of potentially infectious secretions into the lungs, thereby lowering the risk of VAP. The Microcuff ET’s unique cuff is made of an advanced microthin polyurethane material that allows the channels formed upon cuff inflation to ‘self-seal’ within the trachea, increasing protection against fluid leakage into the lungs. In addition, the KimVent Microcuff Endotracheal Tube has a longer length and cylindrical shape cuff, which provides better contact with the tracheal contour and increases protection against fluid leakage. | |||
| The Journal of Critical Care published in its June 2011 edition the findings of a clinical study on mechanical ventilation titled, "A Polyurethane Cuffed Endotracheal Tube is Associated with Decreased Rates of Ventilator-associated Pneumonia" found that VAP rates decreased from 5.3 per 1,000 ventilator days before the use of the polyurethane-cuffed endotracheal tube to 2.8 per 1,000 ventilator days during the intervention year. | ||||
| One way to prevent VAP is to avoid the use of endotracheal tubes altogether. "VAP, or ventilator associated pneumonia, has been referred to as endotracheal tube-associated pneumonia because the ET tube keeps the glottis open and allows secretions from the mouth to enter the lung. "Noninvasive ventilation eliminates problems associated with the endotracheal tube because ventilation is accomplished through a mask interface." | ||||
 | ||||
| Philips Respironics AF531 noninvasive ventilation masks | ||||
| "The avoidance of invasive ventilation is the best way to avoid VAP and all of CareFusion’s conventional ventilators feature this capability," said Ross. "Additionally, the ability to move the patient and the ventilator simultaneously may reduce the manipulation and forces placed on the endotracheal tube during patient transport and thereby may help reduce the occurrence of microaspiration. Again all of CareFusion’s conventional ventilators can be equipped with battery operated compressors to facilitate such movement." | ||||
| Ref: | ||||
| 1. Results are based on a European Multicenter Randomized Trial with 144 patients demonstrating improved respiratory condition, with stable hemodynamic and neurologic status, and no ARDS prior to initiating weaning. Reference: [14] Lelloche et al.; Am J Respir Crit Care Med Vol 174, pp 894-900, 2006 | ||||
| 2. AARP. Fixing to Stay: A National Survey of Housing and Home Modification Issues. May 2000. | ||||
| 3. Linde-Zwirble WT, Bloom JD, Mecca RS, Hansell DM. Post-operative pulmonary complications in the US. Presented at: International Anesthesia Research Society (IARS) annual meeting. March 20-23, 2010; Honolulu, Hawaii. Anes Analg 2010:S-142. | ||||
| 4. Lawrence VA, Hilsenbeck SG, Mulrow CD, Dhanda R, Sapp J, Page CP. Incidence and hospital stay for cardiac and pulmonary complications after abdominal surgery. J Gen Intern Med. 1995;10(12):671-678. | ||||
| 5. Shander A, Fleisher LA, Barie PS, Bigatello LM, Sladen RN, Watson CB. Clinical and economic burden of postoperative pulmonary complications: patient safety summit on definition, risk-reducing interventions, and preventive strategies. Crit Care Med. 2011;39(9):2163-2172. | ||||
| 6. FDA 510(k) clearance. | ||||
| 7. Dezfulian C, Shojania K, Collard HR, Kim HM, Matthay MA, Saint S. Subglottic secretion drainage for preventing ventilator-associated pneumonia: a meta-analysis. Am J Med. 2005;118:11-18. | ||||
| 8. Mujica-Lopez KI, Pearce MA, Narron KA, Perez J, Rubin BK. In vitro evaluation of endotracheal tubes with intrinsic suction. Chest. 2010;138:863-869. | ||||
| Source: | ||||
| Health Care Purchasing News | ||||
| 'Surgical Apgar' Score Can Predict Postop Complications | ||||
 |
||||
| In 1953, Virginia Apgar introduced a 10-point scoring system for evaluation of the condition of newborns, which revolutionized obstetric care. | ||||
| Similar to obstetrics in 1953, surgery today is without a routine and reliable gauge of overall patient condition after surgical procedures to guide clinical practice. | ||||
| The APACHE score and the Physiologic and Operative Severity Score (POSSUM) for the Enumeration of Mortality and Morbidity have both been proposed as clinical measures of patient condition. These scores are not easily calculated at the bedside, require numerous data elements, and rely on laboratory data that are not uniformly collected. As a result, neither has come into standard use for surgical patients. | ||||
| Anesthesiologists Aldrete and Kroulik developed a commonly used, 10-point Postanesthetic Recovery Score to guide discharge from the recovery room, but it was not designed to provide a validated prediction of the risk of major postoperative complications or evaluation of surgical outcome. | ||||
| Atul A Gawande derived a surgical score in a retrospective analysis of data from medical records and the National Surgical Quality Improvement Program for 303 randomly selected patients undergoing colectomy at Brigham and Women’s Hospital, Boston. The primary outcomes measure was incidence of major complication or death within 30 days of operation. | ||||
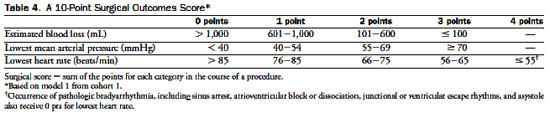
| A 10-point score “surgical Apgar” based on a patient’s estimated amount of blood loss, lowest heart rate, and lowest mean arterial pressure during general or vascular operations was significantly associated with major complications or death within 30 days. | ||||
| 3.8% patients had a surgical score ≤ 4 (bad…) | ||||
| 59% had major complications or died within 30 days after surgery | ||||
| 29% patients had a surgical score ≥ 9 (good…) | ||||
| 4% had major complications or died within 30 days after surgery | ||||
| Among the advantages of using a surgical Apgar score are the patient’s score is computed in the operating room using estimated blood loss, lowest mean arterial pressure, and lowest heart rate. | ||||
 |
||||
| Reynolds et al. perform an invaluable service in validating the score across a vast cohort of operations—123,864 procedures in all. In parallel to the Apgar score, the authors establish that there is strong correlation with mortality, in this case across a variety of surgical subspecialties. Even among specialties with weaker correlations, each point in increase in the Surgical Apgar Score corresponded to a reduction in odds of mortality of 30% or more. | ||||
| So why has it not been adopted in practice? | ||||
| The major reason the Surgical Apgar Score is not used is that surgeons and anesthesiologists believe that their subjective impressions of patient condition are accurate—or at least no less accurate than this simplistic quantitative score. The next needed study is therefore one comparing the accuracy of clinical assessment of patients' postsurgical risk of mortality and morbidity with that of the Surgical Apgar Score. | ||||
| Reference: | ||||
| 1. Atul A. Gawande, MD, MPH, FACS et al. An Apgar Score for Surgery. Journal of the American College of Surgeons Volume 204, Issue 2 , Pages 201-208, February 2007. | ||||
| 2.Critical Need for Objective Assessment of Postsurgical Patients Anesthesiology: June 2011 - Volume 114 - Issue 6 - pp 1269-1270 Editorial Views | ||||
| 3. Reynolds PQ, Sanders NW, Schildcrout JS, Mercaldo ND, St. Jacques PJ: Expansion of the surgical Apgar Score across all surgical subspecialties as a means to predict postoperative mortality. Anesthesiology 2011; 114:1305–12. | ||||
| 4. Does the Surgical Apgar Score Measure Intraoperative Performance? Ann Surg. 2008 August ; 248(2): 320–328 | ||||
| What size endotracheal tube? | |||||||||||||||||||
 |
|||||||||||||||||||
| A quick search on pubmed for “endotracheal tube size sore throat” reveals some interesting reading. | |||||||||||||||||||
| Sore throat is a common postoperative complaint, occurring most often following tracheal intubation. After tracheal intubation, the incidence of sore throat varies from 14.4% to 50% and after laryngeal mask insertion from 5.8% to 34%. | |||||||||||||||||||
| Factors such as tracheal-tube size and cuff design have been shown to be important causative factors. Careful insertion techniques for both the tracheal tube and laryngeal mask are of paramount importance in the prevention of airway trauma and postoperative sore throat. | |||||||||||||||||||
| A 1987 paper by a Seattle based group published in Anesthesiology1 compared use of large tubes (9 for men, 8.5 for women – that’s really large!) or small tubes (7 and 6.5) in 101 adults. The percentage with sore throat afterwards (large vs small) were 45% vs 22% for men (p< 0.02), 53% vs 22% for women (p< 0.05), and 48% vs 22% overall (p< 0.002). They commented that no complications or difficulties were encountered with the smaller tubes. | |||||||||||||||||||
| It has been clearly demonstrated that the use of a smaller tracheal tube reduces the incidence of sore throat, presumably because of decreased pressure at the tube–mucosal interface3 | |||||||||||||||||||
| The Brandt Anaesthesia Tube is designed to prevent intracuff pressure from increasing above 25 mmHg (33 cmH2O), by virtue of the cuff communicating through the inflation line with a pilot balloon that is more compliant and of higher volume. The incidence of postoperative sore throat in patients intubated with this new tube (15%) was significantly lower than that after intubation with a standard Mallinckrodt tube (60%). | |||||||||||||||||||
 |
|||||||||||||||||||
| The cuff seal point should be carefully determined after tracheal intubation and that the intermittent measurement and adjustment of cuff pressure should be routine clinical practice. | |||||||||||||||||||
| Alternatively, simple measures such as inflating the cuff with gas drawn from the breathing circuit or with saline will avoid the problem of N2O diffusion. | |||||||||||||||||||
| There was a higher incidence of sore throat when all the cuffed tubes were lubricated with lignocaine ointments, as opposed to a water-soluble jelly or no lubricant at all. There is no study therefore that categorically demonstrates that the use of lubricating jelly containing a local anaesthetic is beneficial in the reduction of postoperative sore throat after tracheal intubation. | |||||||||||||||||||
| Means of reducing of the incidence of postoperative throat symptoms | |||||||||||||||||||
|
|||||||||||||||||||
| Treatment of postoperative throat symptoms | |||||||||||||||||||
| In most cases, postoperative throat complaints resolve spontaneously without specific treatment. In moderate to severe cases it may be beneficial to treat pain and dysphagia with a gargle containing a drug such as benzydamine hydrochloride, which is approved for the symptomatic treatment of acute sore throat pain. Benzydamine hydrochloride is a topical nonsteroidal anti-inflammatory agent that also has local anaesthetic activity. It has an alkaline pH, which means that it becomes concentrated in inflamed tissue and has minimal systemic absorption. | |||||||||||||||||||
| A much more recent paper from Sweden confirms this observation2. They randomised 100 women to be intubated with either a size 7 or size 6 ETT. There was a significant difference in incidence of sore throat between the 2 groups in Post Anaesthesia Care Unit (48.9% vs 20.8%, p< 0.002). This difference did not persist on follow up at 24, 72, or 96h (although the sore throats certainly did!). | |||||||||||||||||||
| So the evidence supports of using a size 6.0 ETT for women at least. Chances are the same would apply for men but the only study is of size 9 vs size 7. Perhaps you could go with 7 for men, 6 for women. | |||||||||||||||||||
| Reference: | |||||||||||||||||||
| 1.Stout DM, Bishop MJ, Dwersteg JF, Cullen BF. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology. 1987 Sep;67(3):419-21 | |||||||||||||||||||
| 2.Jaensson M, Olowsson LL, Nilsson U. Endotracheal tube size and sore throat following surgery: a randomized-controlled study. Acta Anaesthesiol Scand. 2010 Feb;54(2):147-53 | |||||||||||||||||||
| 3.F. E. McHardy,F. Chung. Postoperative sore throat: cause, prevention and treatment. Anaesthesia: Volume 54, Issue 5, pages 444–453, May 1999. | |||||||||||||||||||
| Further reading: | |||||||||||||||||||
| 1. F. Karasawa, T. Okuda et al. Maintenance of stable cuff pressure in the Brandt™ tracheal tube during anaesthesia with nitrous oxide. Br. J. Anaesth. (2002) 89 (2): 271-276. | |||||||||||||||||||
| 2. Karasawa F, Takita A et al. Changes in gas concentrations in the Brandt endotracheal tube cuff during and after anaesthesia with nitrous oxide. Eur J Anaesthesiol. 2003 May;20(5):391-5 | |||||||||||||||||||