| ANAESTHESIA PEARLS |
| Clinical Case Discussion | |||||
| SHOULD YOU CANCEL SURGERY FOR A BLOOD PRESSURE OF 178/108? | |||||
| Clinical Case Discussion | |||||
| Richard Novak, MD is a Stanford physician | |||||
| You are scheduled to anesthetize a 71-year-old male for an arthroscopic rotator cuff repair. His blood pressure when you meet him in pre-op is 178/108 mmHg. The nurses and the surgeon are alarmed. What would you do? | |||||
 |
|||||
| Discussion: | |||||
| You assess the patient carefully. A review of his chart shows he’s been taking anti-hypertensive oral medications for ten years. His current regimen includes daily atenolol, lisinopril, and amlodipine, with his most recent doses taken this morning with a sip of water. He was seen in his internist’s office one week ago, and at that time his blood pressure was 140/88. His cardiac, renal, and neurologic histories are negative. He walks three miles per day. His resting EKG shows left ventricular hypertrophy, and his BUN and creatinine are normal. The patient’s physical exam is unremarkable except that he appears nervous. | |||||
| Should you cancel the case and send him back to his internist to adjust the blood pressure medical therapy regimen? | |||||
| Should you lower his blood pressure acutely with intravenous antihypertensive drugs, and then proceed with the surgery? | |||||
| Hypertension, defined as two or more blood pressure readings greater than 140/90 mm Hg, is a common affliction found in 25% of adults and 70% of adults over the age of 70 (Miller’s Anesthesia, 7th Edition, Chapter 34, Preoperative Evaluation). Over time, hypertension can cause end-organ damage to the heart, arterial system, and kidneys. Hypertensive and ischemic heart disease are the most common types of organ damage associated with hypertension. Anesthesiologists are always wary of cardiac complications in hypertensive patients. | |||||
| Chronic hypertension is a serious health hazard. But what about a single, markedly-elevated blood pressure value prior to elective surgery? Are there any data to guide our decision about whether to proceed with surgery? There are. A 2004 publication by Howell (Howell SJ et al: Hypertension, hypertensive heart disease and perioperative cardiac risk. Br J Anaesth 2004; 92:570-583) is a meta-analysis of 30 studies examining the relationship between hypertensive disease, elevated admission arterial pressure, and perioperative cardiac outcome. This paper found little evidence for perioperative complications in patients with admission arterial pressures of less than 180 mm Hg systolic or 110 mm Hg diastolic. This paper recommends that anesthesia and surgery not be cancelled for blood pressures lower than 180/110 mm Hg. Based on the Howell study, Miller’s Anesthesia recommends that elective surgery be delayed for hypertension until the blood pressure is less than 180/110 mm Hg. | |||||
| Many of you had seen many hypertensive patients who’d presented for surgery with elevated blood pressures, yet whose blood pressure was adequately controlled in clinic. The anxiety and stress of anticipated surgery can elevate blood pressure acutely. If surgery is cancelled because of this hypertension and the patient is referred back to the primary care internist, the blood pressure is often well-controlled in the office setting on the same drug regimen that gave poor blood pressure control on admission to surgery. A primary care provider will be reluctant to add further medications in the office setting if the blood pressure is not elevated in clinic. | |||||
| What about emergency surgery? | |||||
| What if a patient presents for urgent surgery for acute cholecystitis, and his blood pressure is 190/118 mm Hg? For urgent or emergent surgery, consider titrating intravenous antihypertensive drugs such as labetolol (5–10 mg q 5–10 minutes prn) or hydralazine (5–10 mg q 5–10 minutes prn) to decrease blood pressure prior to initiating anesthesia. Because the eventual induction of general anesthesia with intravenous and volatile anesthetics will lower blood pressure by vasodilation and cardiac depression, any pre-induction antihypertensives must be titrated with great care. Once doses of labetolol or hydralazine are injected, there is no way to remove the effect of that drug. For critically ill patients, consider monitoring with an arterial line and infusing a more titratable and short-acting drug such as nitroprusside for blood pressure control. | |||||
| Intra-operative Management | |||||
| Let’s return to the anesthetic for your elective shoulder surgery patient with the blood pressure of 178/108 mmHg. You begin by administering 2 mg of midazolam IV. Three minutes later his blood pressure decreases to 160/95. You anesthetize him with 50 micrograms of fentanyl and 140 mg of propofol IV, and insert a laryngeal mask airway. In the next 20 minutes, while the patient is moved into a lateral position for the surgery, his blood pressure drops to 95/58. Because most anesthetics depress blood pressure by vasodilation or cardiac depression, it’s common for patients such as this one to require intermittent vasopressors to avoid hypotension, especially at moments when surgical stimulus is minimal. One of the recommendations of the Howell study is that intraoperative arterial pressure be maintained within 20% of the preoperative arterial pressure. This recommendation can be a challenge, especially if the preoperative blood pressure was elevated. A 20% reduction from 178/108 (mean pressure = 131 mm Hg) would be 146/88. A 20% reduction from the mean pressure of 131 mm Hg would be a mean pressure of 104 mm Hg. You choose to treat the patient’s hypotension with 10 mg of IV ephedrine, which raises the blood pressure to 140/85. Fifteen minutes later, the surgeon makes his incision, and the blood pressure escalates to 180/100. You treat this by deepening anesthesia with small, incremental doses of fentanyl and propofol. The surgery concludes, you awaken the patient without complications, and his blood pressure in the Post Anesthesia Care Unit is 150/88 mm Hg. | |||||
| This pattern of perioperative blood pressure lability is common in hypertensive patients, and will require your vigilance to avoid extremes of hypotension or hypertension. Remember that based on the Howell study, Miller’s Anesthesia recommends elective surgery be delayed for hypertension until the blood pressure is less than 180/110 mm Hg. Armed with this information, you’ll cancel fewer patients for preoperative hypertension. | |||||
| Source : | |||||
| theanesthesiaconsultant, Richard Novak, MD. | |||||
| The iControl-RP - Anesthesia robot | |||||||||||||||||
| Richard Novak, MD is a Stanford physician | |||||||||||||||||
| Is this true? Are anesthesiologists on the verge of being replaced by a new robot? | |||||||||||||||||
| The new device being discussed is the iControl-RP anesthesia robot. | |||||||||||||||||
| Closed Loop System | |||||||||||||||||
| In recent years there have been significant advances in the automated delivery of the intravenous anesthetic drugs propofol and remifentanil. (Orliaguet GA, Feasibility of closed-loop titration of propofol and remifentanil guided by the bispectral monitor in pediatric and adolescent patients: a prospective randomized study, 2015 Apr;122(4):759-67). Propofol is an ultra-short-acting hypnotic drug that causes sleep. Remifentanil is an ultra-short-acting narcotic that relieves pain. Administered together, these drugs induce what is referred to as Total Intravenous Anesthesia, or TIVA. Total Intravenous Anesthesia is a technique anesthesiologists use when they choose to avoid using inhaled gases such as sevoflurane and nitrous oxide. Anesthesiologists administer TIVA by adjusting the flow rates on two separate infusion pumps, one infusion pump containing each drug. | |||||||||||||||||
| A closed-loop system is a machine that infuses these drugs automatically. These systems include several essential items: The first is a processed electroencephalogram (EEG) such as a bi-spectral monitor (BIS monitor) attached to the patient’s forehead which records a neurologic measure of how asleep the patient is. The BIS monitor calculates a score between 0 and 100 for the patient’s level of unconsciousness, with a score of 100 corresponding to wide awake and 0 corresponding to a flat EEG. A score of 40 – 60 is considered an optimal amount of anesthesia depth. The second and third essential items of a closed-loop automated system are two automated infusion pumps containing propofol and remifentanil. A computer controls the infusion rate of a higher or lower amount of these drugs, depending on whether the measured BIS score is higher or lower than the 40- 60 range. | |||||||||||||||||
| iControl RP | |||||||||||||||||
| Researchers in Canada have expanded this technology into a device they call the iControl-RP, which is in clinical trials at the University of British Columbia. The iControl-RP is a closed-loop system which makes its own decisions. The initials RP stand for the two drugs being titrated: remifentanil and propofol. In addition to monitoring the patient’s EEG level of consciousness (via a BIS monitor device called NeuroSENSE), this new device monitors traditional vital signs such as blood oxygen levels, heart rate, respiratory rate, and blood pressure, to determine how much anesthesia to deliver. | |||||||||||||||||
| Clinical Trials | |||||||||||||||||
| Per published information on their research protocol, the iControl-RP allows either remifentanil or propofol to be operated in any of three modes: (1) closed-loop control based on feedback from the EEG as measured by the NeuroSENSE; (2) target-controlled infusion (TCI), based on previously-described pharmacokinetic and pharmacodynamic models; and (3) conventional manual infusion, which requires a weight-based dose setting. (Reference: Closed-loop Control of Anesthesia: Controlled Delivery of Remifentanil and Propofol Dates, Status, Enrollment Verified by: Fraser Health, August 2014, First Received: January 15, 2013, Last Updated: March 5, 2015, Phase: N/A, Start Date: February 2013, Overall Status: Recruiting, Estimated Enrollment: 150). | |||||||||||||||||
| In Phase 1 of the iControl-RP testing involving 50 study subjects, propofol will be administered in closed-loop mode and a remifentanil infusion will be administered based on a target-controlled infusion. In phase 2 involving 100 study subjects, both propofol and remifentanil will be administered in closed-loop mode. The investigators aim to demonstrate that closed-loop control of anesthesia and analgesia based on EEG feedback is clinically feasible. | |||||||||||||||||
| In both phases, an anesthesiologist will monitor the patient as per routine practice and have the ability to modify the anesthetic or analgesic drugs being administered. That is, he or she will be able to adjust the target depth of hypnosis, adjust the target effect site concentration for remifentanil, immediately switch to manual control of either infusion, administer a bolus dose, or immediately stop the infusion of either drug. iControl-RP is connected to the NeuroSENSE EEG monitor, the two infusion pumps for separately controlled propofol and remifentanil administration, and the operating room patient vital signs monitor. A user interface allows the anesthesiologist to set the target EEG depth level, switch between modes of operation (manual, target-controlled infusion, or closed-loop), and set manual infusion rates or target effect-site concentrations for either drug as required. | |||||||||||||||||
| Per the article in the Washington Post. (Todd C. Frankel, Washington Post, May 15, 2015), one of the machine’s co-developers Mark Ansermino, MD said, “We are convinced the machine can do better than human anesthesiologists.” The iControl-RP has been used to induce deep sedation in adults and children undergoing general surgery. The device had been used on 250 patients so far. | |||||||||||||||||
| Why is this robotic device only a small step toward replacing anesthesiologists? | |||||||||||||||||
| A critical realization is that anesthetizing patients requires far more skill than merely titrating two drug levels. Every patient requires... | |||||||||||||||||
|
|||||||||||||||||
| In the future, closed-loop titration of drugs may lessen an anesthesiologist’s workload and free him or her for other activities. In the distant future, closed-loop titration of drugs may free a solitary anesthesiologist to initiate and monitor multiple anesthetics simultaneously from a control booth via multiple video screens and interface displays. But the handling of all tasks (1) – (6) by an automated robotic device is still the stuff of science fiction. The Washington Post article said an early role for the machine could be in war zones or remote areas where an anesthesiologist is unavailable. One could conjecture that a closed-loop anesthesia system may be used to facilitate surgery in outer space some day as well. | |||||||||||||||||
| In either case, an anesthesiologist or some other highly-trained medical professional will still be required on site to achieve tasks (1) – (6). | |||||||||||||||||
| The iControl-RP has not been approved by the U.S. Food and Drug Administration. | |||||||||||||||||
| The iControl-RP team has struggled to find a corporate backer for its project. Dr. Ansermino, the anesthesiologist inventor in Vancouver, told the Washington Post, “Most big companies view this as too risky,” but he believed a device like this was inevitable. “I think eventually this will happen,” Ansermino told the Washington Post, “whether we like it or not.” | |||||||||||||||||
| Source : | |||||||||||||||||
| theanesthesiaconsultant, Richard Novak, MD. | |||||||||||||||||
| ANESTHESIOLOGY PRACTICE | |||||
| THE TOP 10 MOST STRESSFUL SITUATIONS IN ANESTHESIOLOGY PRACTICE | |||||
| Richard Novak, MD is a Stanford physician | |||||
| 10. Emergency general anesthesia in a morbidly obese patient | |||||
| Picture a 350-pound man with a bellyful of beer and pizza, who needs an emergency general anesthetic. When a patient with a Body Mass Index (BMI) > 40 needs to be put to sleep urgently, it’s dangerous. Oxygen reserves are low in a morbidly obese patient, and if the anesthesiologist is unable to place an endotracheal tube safely, there’s a genuine risk of hypoxic brain damage or cardiac arrest within minutes. | |||||
 |
|||||
| 9. Liver transplantation | |||||
| Picture a patient ill with cirrhosis and end-stage-liver-failure who needs a complex 10 to 20-hour-long abdominal surgery, a surgery which frequently demands massive transfusion equal to one blood volume (5 liters) or more. These cases are maximally stressful in both intensity and duration. | |||||
 |
|||||
| 8. An emergency Cesarean section under general anesthesia in the wee hours of the morning | |||||
| Picture a 3 a.m. emergency general anesthetic on a pregnant woman whose fetus is having cardiac decelerations (a risky slow heart rate pattern). The anesthesiologist needs to get the woman to sleep within minutes so the baby can be delivered by the obstetrician. Pregnant women have full stomachs and can have difficult airway because of weight changes and body habitus changes of term pregnancy. If the anesthesiologist mismanages the airway during emergency induction of anesthesia, both the mother and the child’s life are in danger from lack of oxygen within minutes. | |||||
 |
|||||
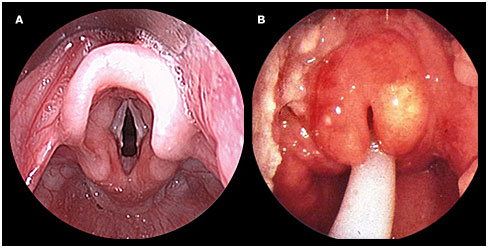
| 7. Acute epiglottitis in a child | |||||
| Picture an 11-month-old boy crowing for every strained breath because the infection of acute epiglottis has caused swelling of his upper airway passage. These children arrive at the Emergency Room lethargic, gasping for breath, and turning blue. Safe anesthetic management requires urgently anesthetizing the child with inhaled sevoflurane, inserting an intravenous line, and placing a tracheal breathing tube before the child’s airway shuts down. A head and neck surgeon must be present to perform an emergency tracheostomy should the airway management by the anesthesiologist fails. | |||||
 |
|||||
| 6. Any emergency surgery on a newborn baby | |||||
| Picture a one-pound newborn premature infant with a congenital defect that is a threat to his or her life. This defect may be a diaphragmatic hernia (the child’s intestines are herniated into the chest), an omphalocele (the child’s intestines are protruding from the anterior abdominal wall, spina bifida (a sac connected to the child’s spinal cord canal is open the air through a defect in the back), or a severe congenital heart disorder such as a transposition of the great vessels (the major blood vessels: the aorta, the vena cavas and the pulmonary artery, are attached to the heart in the wrong locations). Anesthetizing a patient this small for surgeries this big requires the utmost in skill and nerve. | |||||
 |
|||||
| 5. Acute anaphylaxis | |||||
| Picture a patient’s blood pressure suddenly dropping to near zero and their airway passages constricting in a severe acute asthmatic attack. Immediate diagnosis is paramount, because intravenous epinephrine therapy will reverse most anaphylactic insults, and no other treatment is likely to be effective. | |||||
 |
|||||
| 4. Malignant Hyperthermia | |||||
| Picture an emergency where an anesthetized patient’s temperature unexpectedly rises to over 104 degrees Fahrenheit due to hypermetabolic acidotic chemical changes in the patient’s skeletal muscles. The disease requires rapid diagnosis and treatment with the antidote dantrolene, as well as acute medical measures to decrease temperature, acidosis, and high blood potassium levels which can otherwise be fatal. | |||||
 |
|||||
| 3. An intraoperative myocardial infarction (heart attack) | |||||
| Picture an anesthetized 60-year-old patient who develops a sudden drop in their blood pressure due to failed pumping of their heart. This can occur because of an occluded coronary artery or a severe abnormal rhythm of their heart. Otherwise known as cardiogenic shock, this syndrome can lead to cardiac arrest unless the heart is supported with the precise correct amount of medications to increase the pumping function or improve the arrhythmia. | |||||
 |
|||||
| 2. Any massive trauma patient with injuries both to their airway and to their major vessels | |||||
| Picture a motorcycle accident victim with a bloodied, smashed-in face and a blood pressure of near zero due to hemorrhage. The placement of an airway tube can be extremely difficult because of the altered anatomy of the head and neck, and the management of the circulation is urgent because of the empty heart and great vessels secondary to acute bleeding. | |||||
 |
|||||
| 1. The syndrome of “can’t intubate, can’t ventilate | |||||
| ” You’re the anesthesiologist. Picture any patient to whom you’ve just induced anesthesia, and your attempt to insert the tracheal breathing tube is impossible due to the patient’s anatomy. Next you attempt to ventilate oxygen into the patient’s lungs via a mask and bag, and you discover that you are unable to ventilate any adequate amount of oxygen. The beep-beep-beep of the oxygen saturation monitor is registering progressively lower notes, and the oximeter alarms as the patient’s oxygen saturation drops below 90%. If repeated attempts at intubation and ventilation fail and the patient’s oxygen saturation drops below 85-90% and remains low, the patient will incur hypoxic brain damage within 3 – 5 minutes. This situation is the worst-case scenario that every anesthesia professional must avoid if possible. If it does occur, the anesthesia professional or a surgical colleague must be ready and prepared to insert a surgical airway (cricothyroidotomy or tracheostomy) into the neck before enough time passes to cause irreversible brain damage. | |||||
 |
|||||
| Source : | |||||
| theanesthesiaconsultant, Richard Novak, MD. | |||||
