| ANAESTHESIA PEARLS |
- Transesophageal Echocardiography in Cardiac Arrest
- Care CMQCC OB HEMORRHAGE CARE GUIDELINES FLOW CHART
- Cheating death through 'suspended animation'
| By Stephen Alerhand MD, Resident Physician, Icahn School of Medicine at Mount Sinai | ||||||||||||||||||||||||||||||||||||||
|
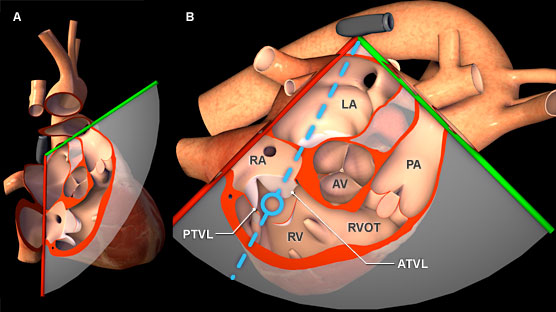
Transesophageal echocardiography (TEE or TOE) used to be the domain of cardiologists. It has lately seeped into other areas of medicine where hemodynamic evaluation is crucial. ICU's and occasionally OR's use them even for non-cardiac surgery. But the TEE probe can quite easily be used in any unconscious, intubated patient. One obvious indication would be cardiac arrests. With the TEE probe indwelling, you can evaluate the quality of the compressions, and you get minimal hands-off time for evaluating cardiac contractility, cardiac filling and any signs of other pathology like pulmonary embolism, pericardial effusions etc. to sign off your H&T's. | ||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
| TEE in cardiac arrest | ||||||||||||||||||||||||||||||||||||||
| According to the 2008 ACEP Ultrasound Guidelines, as well as Matt and Mike from the Ultrasound podcast, that emerging emergency ultrasound application is…Transesophageal echocardiography (TEE) in cardiac arrest. | ||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
| Absolute Contraindications | ||||||||||||||||||||||||||||||||||||||
| Perforated viscous, esophageal pathology or esophagectomy, UGI bleed or recent UGI surgery | ||||||||||||||||||||||||||||||||||||||
| Relative Contraindications | ||||||||||||||||||||||||||||||||||||||
| Cervical spine disease, hiatal hernia, coagulopathy, prior chest radiation | ||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||
| Specific Applications of TEE in Cardiac Arrest | ||||||||||||||||||||||||||||||||||||||
| Blaivas, Michael. Transesophageal echocardiography during cardiopulmonary arrest in the emergency department. Resuscitation 78 (2008): 135-140. | ||||||||||||||||||||||||||||||||||||||
| Brief description of 6 applications described in this paper: | ||||||||||||||||||||||||||||||||||||||
| Case 1:TTE (Trans Thoracic Echo) showed no cardiac motion. TEE did. Compressions halted, pressors started. | ||||||||||||||||||||||||||||||||||||||
| 35M brought in by EMS undergoing CPR… TTE showed limited view but no cardiac motion. No pulses. TEE showed contraction w/ EF 15%. Thus compressions halted. Pressors started. Extubated and released days later. | ||||||||||||||||||||||||||||||||||||||
| Case 2: Monitor showed asystole. TEE showed V-fib and chest compression quality. | ||||||||||||||||||||||||||||||||||||||
| 73 obese F p/w difficulty breathing and hypoxia. Developed tachypnea and decreased alertness. Intubated, then arrested. Monitor showed asystole. Poor images on echo showing cardiac standstill. TEE showed V-fib, thus shock applied. Eventually labs returned with K >9. Hyperkalemia meds given. Providers giving compressions rotated in based upon inadequate compressions on TEE. Eventually developed EF >50%. | ||||||||||||||||||||||||||||||||||||||
| Case 3: TTE showed standstill. TEE showed Vent fib and thrombus. Given tPA. | ||||||||||||||||||||||||||||||||||||||
| 73F p/w sudden-onset SOB, collapsed, intubated in field. ROSC prior to arrival. Echo showed cardiac standstill. Pulses present. Monitor showed heart beat. TEE showed cardiac standstill, thus CPR restarted. Then showed V-fib, thus patient shocked into ROSC. TEE also showed thrombus leaving RA and entering RV, thus given tPA bolus and started on Heparin. | ||||||||||||||||||||||||||||||||||||||
| Case 4: TTE showed standstill. TEE showed PICC line catheter tip striking RA. PICC line pulled back. | ||||||||||||||||||||||||||||||||||||||
| 45M receiving Abx through PICC line collapsed shortly after infusion. EMS found in V-fib, CPR started. No pulses. Echo showed standstill. TEE showed V-fib along with catheter tip in entrance to RA periodically striking wall. Thus PICC line pulled back. | ||||||||||||||||||||||||||||||||||||||
| Case 5: TTE showed asystole. TEE showed no RV strain, but rather aortic dissection. TPA held, Thoracic Surg called in. | ||||||||||||||||||||||||||||||||||||||
| 37M PMH DVT and PE 2/2 hypercoagulability disorder c/o cp. Arrested in ED. Echo showed asystole. No pulses. Presumptive diagnosis of PE made. TEE showed no RV strain or ventricular septal movement abnormalities, but rather proximal aortic dissection. TPA thus cancelled, Thoracic Surgery called in for aortic graft placement. | ||||||||||||||||||||||||||||||||||||||
| Case 6:TTE suggested acute PE. TEE showed chronic process. TPA held. | ||||||||||||||||||||||||||||||||||||||
| 61F collapsed at home after c/o sob. Pulses lost en route, V-fib, shocked into PEA. Echo showed myocardial contractions with severely depressed function, RA and RV dilation, images limited 2/2 body habitus and emphysema. Monitor showed V-fib, patient shocked. TEE showed minimal R heart strain and no paradoxical movement of septum into LV, consistent w/ chronic RA and RV dilation. No thrombus seen. TPA held. | ||||||||||||||||||||||||||||||||||||||
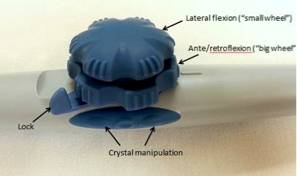
| Performing TEE in Cardiac Arrest | ||||||||||||||||||||||||||||||||||||||
| • TEE probe inserted into esophagus, using laryngoscopy if needed | ||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
| • Controls on handle allow manipulation of US beam for array of visual orientations of heart | ||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||
| • Maximal penetrating depth of 19-20 cm, with high frequency. | ||||||||||||||||||||||||||||||||||||||
| Source: | ||||||||||||||||||||||||||||||||||||||
| Transesophageal Echocardiography in Cardiac Arrest. By Stephen Alerhand MD Resident Physician, Icahn School of Medicine at Mount Sinai. Edited by Alex Koyfman MD. www.emdocs.net | ||||||||||||||||||||||||||||||||||||||
| Reference: | ||||||||||||||||||||||||||||||||||||||
|
Transesophageal echocardiography during cardiopulmonary arrest in the emergency department, Resuscitation, 2008. The usefulness of transesophageal echocardiography during intraoperative cardiac arrest in noncardiac surgery, Anesth Analg, 2006. Diagnostic accuracy of transesophageal echocardiography during cardiopulmonary resuscitation, J Am Coll Cardiol, 1997. Emergent limited perioperative transesophageal echocardiography: should new guidelines exist for limited echocardiography training for anesthesiologists? Front Med, 2012. | ||||||||||||||||||||||||||||||||||||||
| Ultrasound guided CPR | ||||||||||||||||||||||||||||||||||||||
| Part1: | ||||||||||||||||||||||||||||||||||||||
| Part2: | ||||||||||||||||||||||||||||||||||||||
| By California Maternal Quality Care Collaborative. ( CMQCC) | |||||
| Stage 1 : OB Hemorrhage | |||||
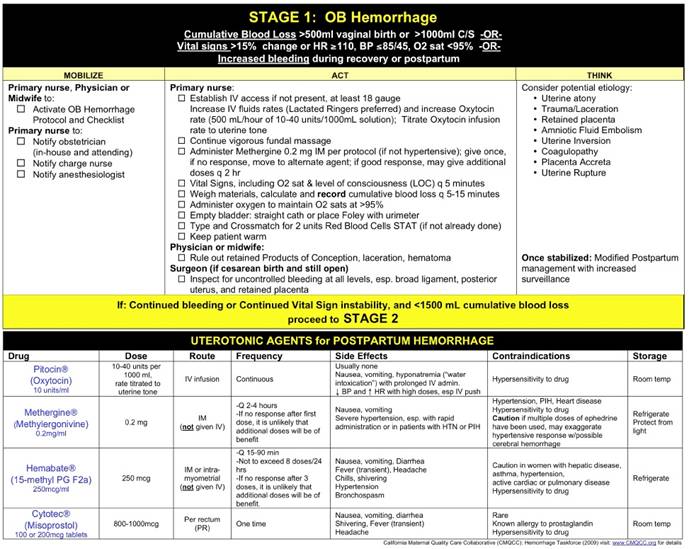 |
|||||
| Stage 2 : OB Hemorrhage | |||||
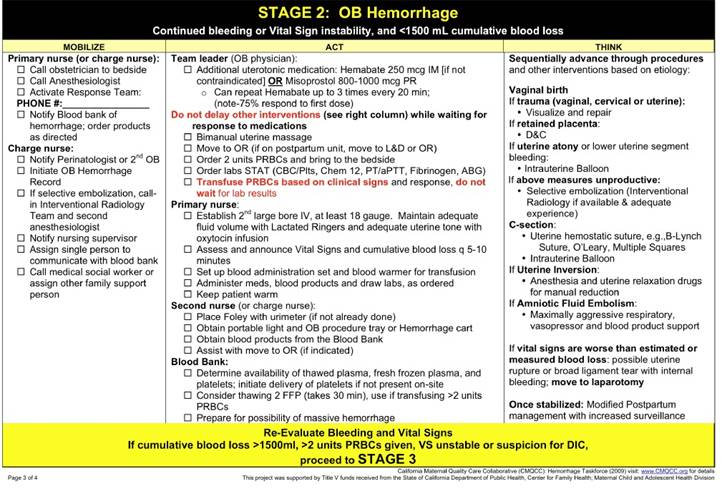 |
|||||
| Stage 3 : OB Hemorrhage | |||||
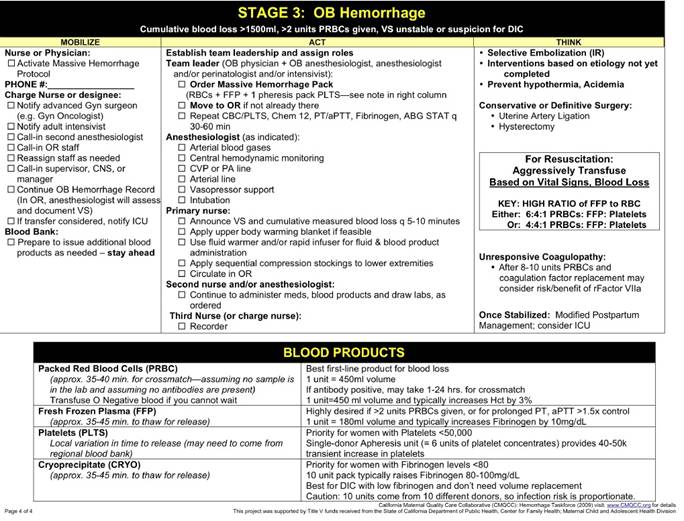 |
|||||
| CMQCC OBHEMORRHAGE CARE GUIDELINES FLOW CHART | |||||
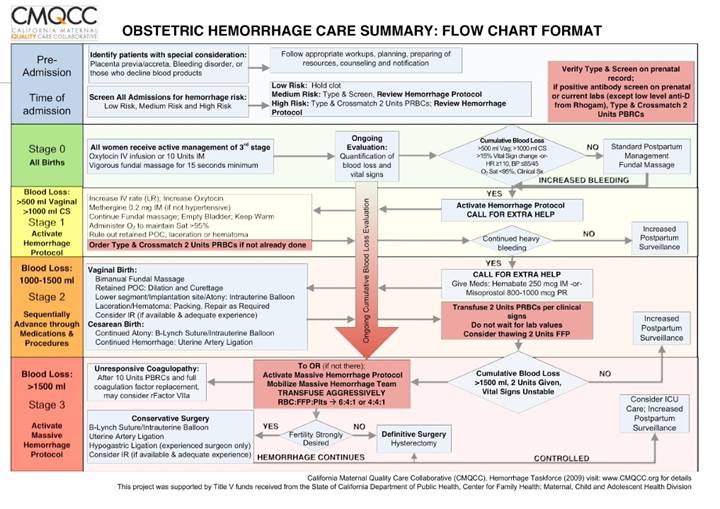 |
|||||
| MQCC OB HEMORRHAGE CARE GUIDELINES TABLE CHART | |||||
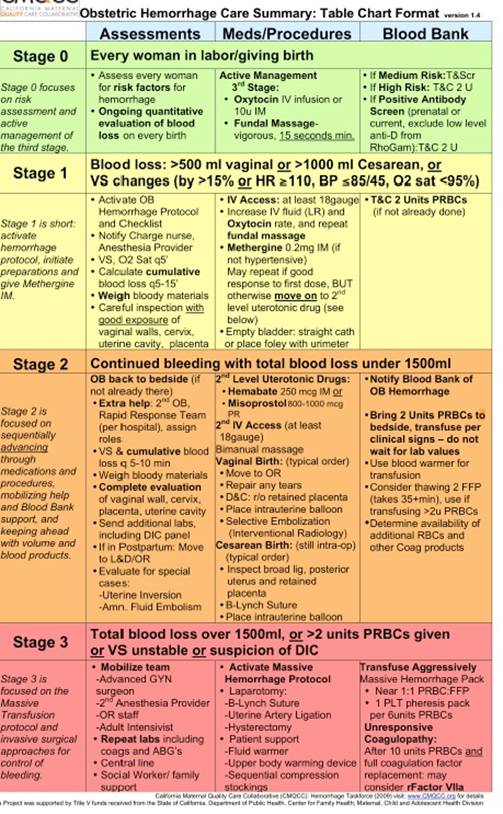 |
|||||
| Going live – on the dead | |||||
|
"When patients have bled so much that the heart stops, we know that we have very little chance of saving them," said veteran trauma surgeon Samuel Tisherman. Even with breathing tubes, IVs and emergency chest surgery, less than one in 10 of such patients survive, he said. "The outcomes are pretty dismal." But Tisherman and a handful of other doctors may have found an innovative way to beat these grim odds. | |||||
 |
|||||
|
"Some people, including us early on ... have called this idea 'suspended animation.' And in some sense, that's true," said Tisherman, who is spearheading a new clinical trial at the UPMC Presbyterian Hospital in Pittsburgh, Pennsylvania. He and his researchers are experimenting with something called induced hypothermia, or cooling trauma patients' bodies to ward off the potential damage caused by loss of blood and oxygen. Because it causes the patient's cell activity to shut down, this method essentially places the person in a sort of temporary limbo -- not dead, but not fully alive, either -- as a way of buying surgeons more time. The team say they're reluctant to use the term suspended animation, as it sounds like a sci-fi movie. They probably have to say that to sound professional, as "Emergency Preservation and Resuscitation," or EPR a new term. Stab or gunshot victims at the edge of life will be rapidly cooled to suspend cell activity to buy time to be and taken to surgery to fix them before rewarming and restarting them. At the edge of life actually means dead? Inclusion is by traumatic cardiac arrest – described as loss of pulse – less than 5 mins before entering the Emergency Department (ED) or in the ED. Then, all standard life saving measures, including thoracotomy must have been performed before suspended animation is initiated. The thoracotomy is also needed to access the aorta for rapid cooling. The trial is run by Dr. Tisherman and a short, but interesting protocol is available at clinicaltrials.gov , and was recently presented in a news article. | |||||
| Inducing suspended animation | |||||
|
The goal is to induce deep hypothermia quickly to avoid hypoxic damage. This is done by rapidly flushing a cold crystalloid solution through the body, replacing all the blood and inducing hypothermic metabolic arrest – or, said in a cooler way, suspended animation. There's been a lot of studying on dogs and pigs, with promising results. Even after being in profound hypovolemic shock for up to one hour before initiation of suspended animation. There have also been studies on different techniques and targets, showing that rapid cooling is beneficial, and that the optimal cooling target apparently is 10 degrees celcius. 15 degrees slightly worse, 5 degrees a lot worse. But all tests are small in numbers. But this is what we have so far, so rapid cooling and 10 degrees is what they're going for in Pittsburgh. Tests have been on anaesthetisted dogs and pigs having inflicted lethal bleeding injuries and then put on suspended animation before exsanguinating to cardiac arrest. True suspended animation is still a dream, as metabolism isn't really arrested, merely slowed down considerably. | |||||
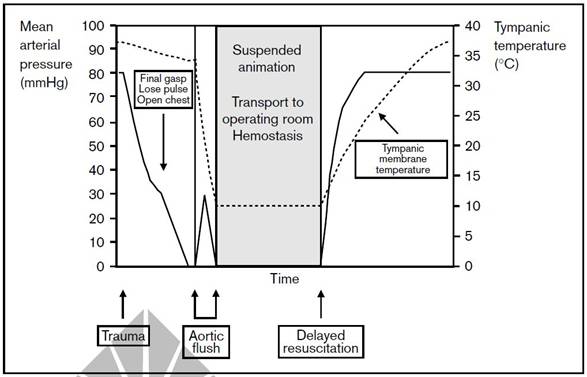 |
|||||
| The goal is survival, including good neurological survival. By clamping the aorta, the cooling first focuses on the upper body, and most importantly, the brain. Neurological tests has been looking at animals retaining previously learned procedures, and how they adapt to learning new stuff. Both these parameters are good with up to 60 minutes in suspended animation, and in some settings up to 90 minutes. 120 minutes seems to be pushing it with current techniques. | |||||
| The Pittsburgh experiment | |||||
|
And now it's been decided the time has come for human tests. It will be interesting to see if quick cooling to suspended animation is feasible in real settings with real humans, and give time and opportunity for surgeons to fix the problem, and then finally wake the persons back up with intact physiology and neurology. | |||||
| Interview with the Pittsburgh team | |||||
| Still, this is not new | |||||
|
Once cooled, the trials have either had subjects on no circulation, or on a low flow external circulation (ie a cardio-pulmonary bypass circuit). For the rewarming, the subjects are put on bypass, crystalloid goes out, blood goes in and is heated through the bypass system. They're in suspended animation., In that setting, they're not much different from thoracic anaesthesia where thoracic aortic surgery is sometimes performed on cooled patients with the heart stopped and no bypass running. This gives the surgeons very limited time to do the repair. Cooling the patient further, and removing the blood, buys a lot of extra time. A similar thing happens with drownings that are 'naturally' cooled before going into arrest. They are in state of suspended animation when they get to hospital and get rewarmed. | |||||
| Other future uses | |||||
|
As mentioned, this treatment buys time, much like ECMO does for heart and/or lung failure, and might not be just for trauma bleedings. Safar mentions in his overview article that "Suspended animation could also be useful when surgeons and anesthesiologists are unexpectedly losing ground with unmanageable hemorrhage during various surgical operations – and for performing otherwise infeasible cardiovascular or neurosurgical procedures." | |||||
| Source: | |||||
| Suspended animation. www.scancrit.com | |||||
| Cheating death through 'suspended animation. By Brandon Griggs, CNN. | |||||
| Reference: | |||||
| There are a lot of available articles on suspended animation, many (most) of them written by Peter Safar and Hasan Alam. First, though, is Tisherman's protocol. Then a nice overview on suspended animation by Safar, followed by one of Alam's experiments: | |||||
|
Emergency Preservation and Resuscitation (EPR) for Cardiac Arrest From Trauma (EPR-CAT), Tisherman, clinicaltrials.gov, 2011. Suspended animation for delayed resuscitation, Safar, Curr Opin Anaesthesiol, 2002. Learning and memory is preserved after induced asanguineous hyperkalemic hypothermic arrest in a swine model of traumatic exsanguination, Alam, Surgery, 2002. | |||||
