| |
ADVANCES AFFECTING ANESTHESIA |
| |
THE TOP TEN MOST USEFUL ADVANCES AFFECTING ANESTHESIA IN THE PAST 25 YEARS |
| |
Richard Novak, M.D.
|
| |
In 1986 the American Society of Anesthesiologists adopted pulse oximetry and end-tidal CO2 monitoring as standards of care. These two monitors were our specialty’s major advances in the 1980’s, and made anesthesia safer for everyone. |
| |
What are the most significant advances affecting anesthesia since that time? |
| |
THE TOP TEN MOST USEFUL ADVANCES AFFFECTING ANESTHESIA IN THE PAST 25 YEARS (1987- 2012): |
| |
#10. The cell phone (replacing the beeper) |
| |
 |
Cell phones changed the world, and they changed anesthesia practice as well. Before the cell phone, you’d get paged while driving home and have to search to find a payphone. Cell phones allow you to be in constant contact with all the nurses and doctors involved in your patient’s care at all times. No one should carry a beeper anymore. |
|
| |
#9. Ultrasound use in the operating room |
| |
| The ultrasound machine aids peripheral nerve blockade and catheter placement, and intravascular catheterization. Nerve block procedures used to resemble “voodoo medicine,” as physicians stuck sharp needles into tissues in search of paresthesias and nerve stimulation. Now we can see what we’re doing. |
 |
|
| |
#8. The video laryngoscope |
| |
 |
Surgeons have been using video cameras for decades. We finally caught up. Although there’s no need for a video laryngoscope on routine cases, the device is an invaluable tool for seeing around corners during difficult intubations. |
|
| |
#7. Rocuronium |
| |
| Anesthesiologists long coveted a replacement for the side-effect-ridden depolarizing muscle relaxant succinylcholine. Rocuronium is not as rapid in onset as succinylcholine, but it is the fastest non-depolarizer in our pharmaceutical drawer. |
 |
|
| |
#6.Ondansetron |
| |
 |
The introduction of ondansetron and the 5-HT3 receptor blocking drugs gave anesthesiologists our first effective therapy to combat post-operative nausea and vomiting. |
|
| |
#5. The Internet |
| |
| The Internet changed the world, and the Internet changed anesthesia practice as well. With Internet access, clinicians are connected to all known published medical knowledge at all times. Doctors have terrific memories, but no one remembers everything. Now you can research any medical topic in seconds. Some academics opine that the use of electronic devices in the operating room is dangerous, akin to texting while driving. Monitoring an anesthetized patient is significantly different to driving a car. Much of O.R. monitoring is auditory. We listen to the oximeter beep constantly, which confirms that our patient is well oxygenated. |
 |
| A cacophony of alarms sound whenever vital signs vary from norms. An anesthesia professional should never let any electronic device distract him or her from vigilant monitoring of the patient. |
|
| |
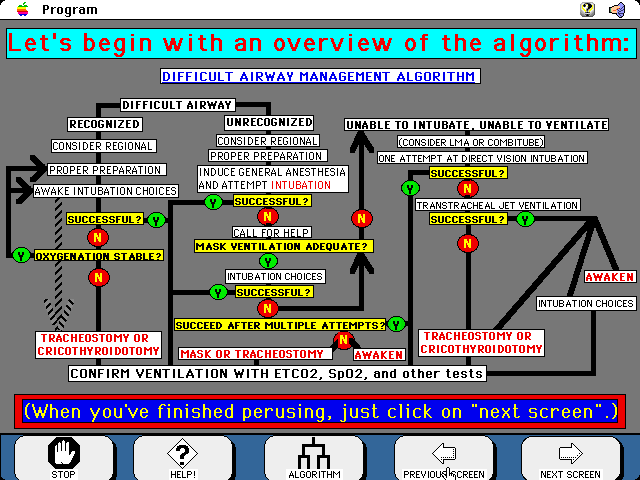
#4. The ASA Difficult Airway Algorithm |
| |
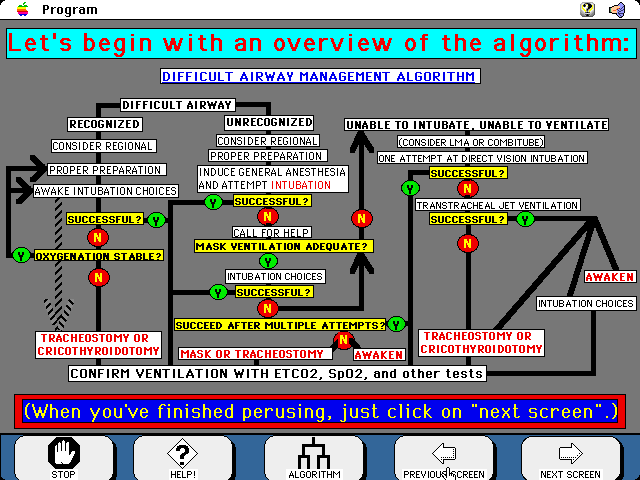 |
Anesthesia and critical care medicine revolve around the mantra of “Airway-Breathing-Circulation.” When the ASA published the Difficult Airway Algorithm in Anesthesiology in 2003, they validated a systematic approach to airway management and to the rescue of failed airway situations. It’s an algorithm that we’ve all committed to memory, and anesthesia practice is safer as a result. |
|
| |
#3. Sevoflurane |
| |
|
Sevo is the volatile anesthetic of choice in community private practice, and is a remarkable improvement over its predecessors. Sevoflurane is as insoluble as nitrous oxide, and its effect dissipates significantly faster than isoflurane. Sevo has a pleasant smell, and it replaced halothane for mask inductions. |
 |
|
| |
#2. Propofol |
| |
 |
Propofol is wonderful hypnotic for induction and maintenance. It produces a much faster wake-up than thiopental, and causes no nausea. Propofol makes us all look good when recovery rooms are full of wide-awake, happy patients. |
|
| |
#1. The Laryngeal Mask Airway |
| |
| What an advance the LMA was. We used to insert endotracheal tubes for almost every general anesthesia case. Endotracheal tubes necessitated laryngoscopy, muscle relaxation, and reversal of muscle relaxation. LMA’s are now used for most extremity surgeries, many head and neck surgeries, and most ambulatory anesthetics. |
 |
|
| |
Ref: |
| |
1.THE TOP TEN MOST USEFUL ADVANCES AND THE FIVE MOST OVERRATED ADVANCES AFFECTING ANESTHESIA IN THE PAST 25 YEARS; Theanesthesiaconsultant Blog |