| |
Guidelines for the management of difficult and failed tracheal intubation in obstetrics |
| |
INTRODUCTION: |
| |
The rate of failed tracheal intubation in obstetrics has remained unchanged over the past four decades. The first obstetric failed intubation guideline was published by Tunstall in 1976.
|
| |
The Obstetric Anaesthetists' Association and Difficult Airway Society have developed the first national obstetric guidelines for the safe management of difficult and failed tracheal intubation during general anaesthesia.
|
| |
WHY IS AIRWAY MANAGEMENT MORE DIFFICULT IN THE OBSTETRIC PATIENT? |
| |
Maternal, fetal, surgical and situational factors contribute to the increased incidence of failed intubation.
|
| |
The mucosa of the upper respiratory tract becomes more vascular and oedematous, leading to increased risk of airway bleeding and swelling. These changes result in increasing Mallampati score as pregnancy progresses, and also during labour and delivery. Swelling may be exacerbated by pre-eclampsia, oxytocin infusion, intravenous fluids and Valsalva manoeuvres during labour and delivery. Decreased functional residual capacity and increased oxygen requirements accelerate the onset of desaturation during apnoea, and these are exacerbated in the obese parturient. Progesterone reduces lower oesophageal sphincter tone, resulting in gastric reflux, and a delay in gastric emptying occurs during painful labour and after opioid administration. Enlarged breasts may make the insertion of the laryngoscope difficult.
|
| |
THE OAA/DAS OBSTETRIC DIFFICULT AND FAILED INTUBATION GUIDELINES |
| |
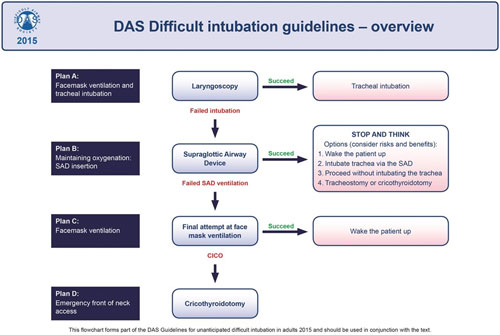
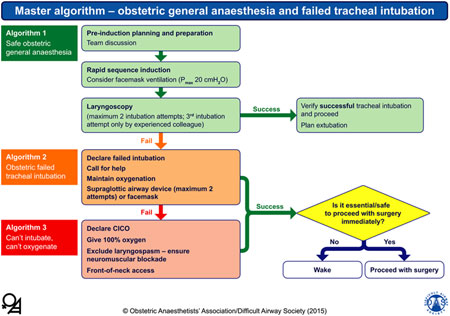
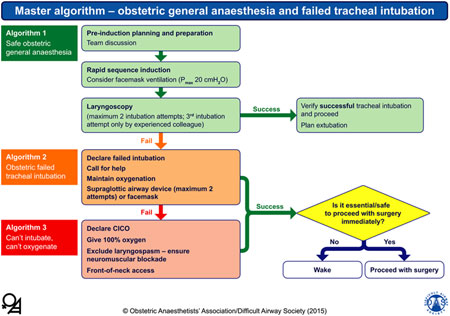
1. Master algorithm – obstetric general anaesthesia and failed tracheal intubation: |
| |
 |
| |
The yellow diamond represents a decision-making step. Pmax, maximal inflation pressure, ; CICO, ‘can't intubate, can't oxygenate’. |
| |
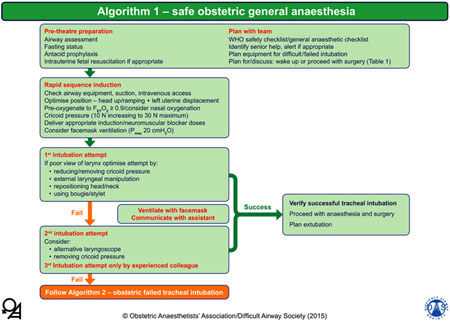
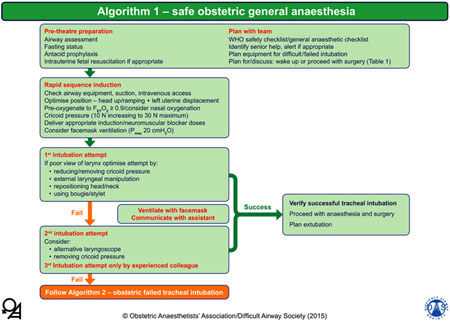
2. Algorithm 1 – safe obstetric general anaesthesia: |
| |
 |
| |
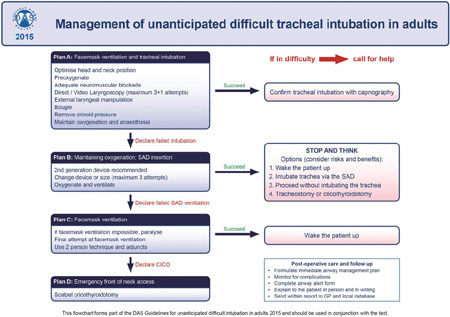
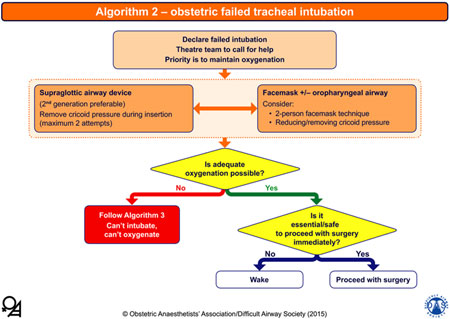
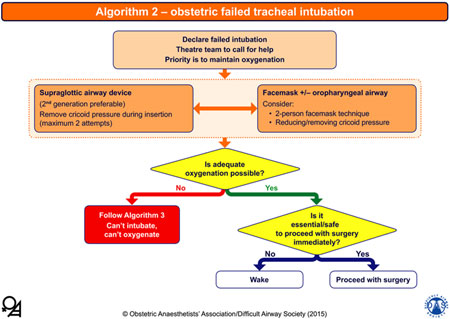
3. Algorithm 2 – obstetric failed tracheal intubation: |
| |
 |
| |
The yellow diamonds represent decision-making steps; the lower right decision step links to Table 1. The boxes at the bottom link to Table 2. |
| |
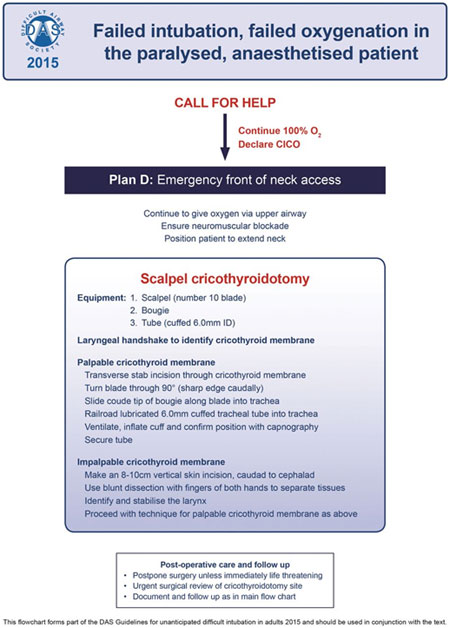
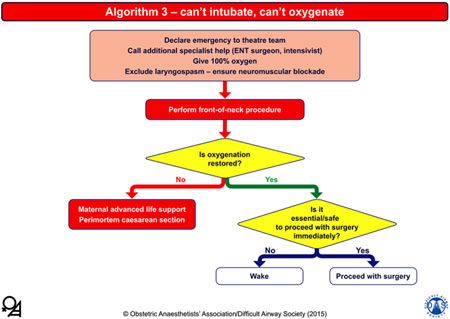
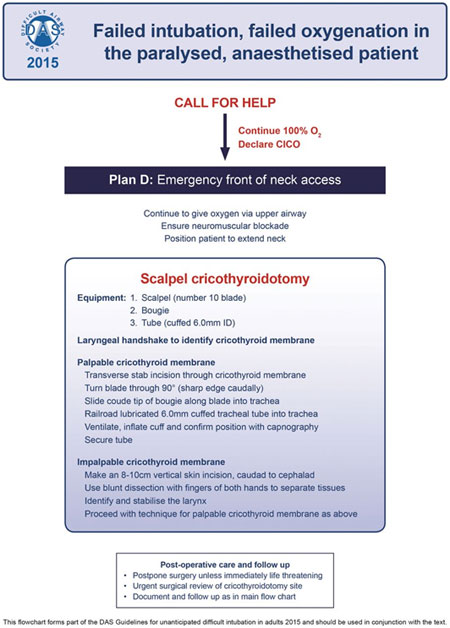
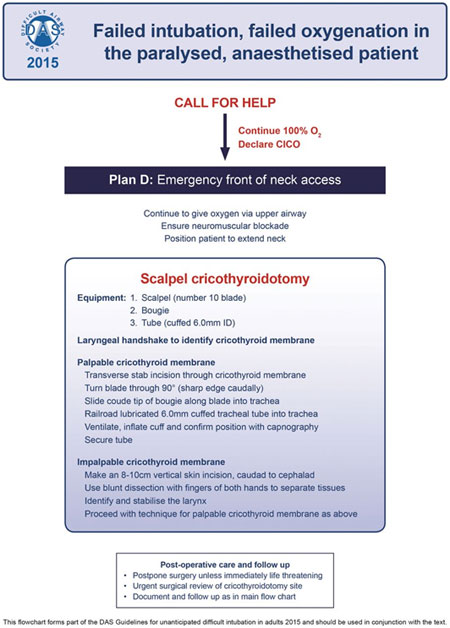
4. Algorithm 3 – can't intubate, can't oxygenate: |
| |
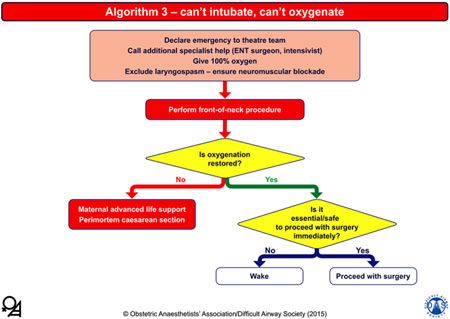 |
| |
The yellow diamonds represent decision-making steps; the lower right decision step links to Table 1. The boxes at the bottom link to Table 2. |
| |
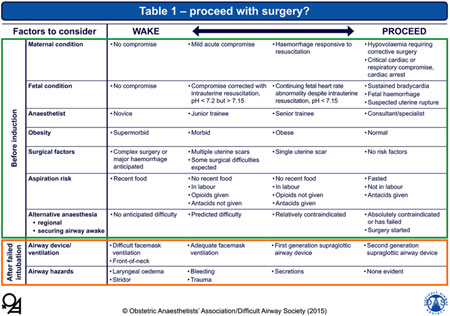
5. Table 1 – wake or proceed to surgery? |
| |
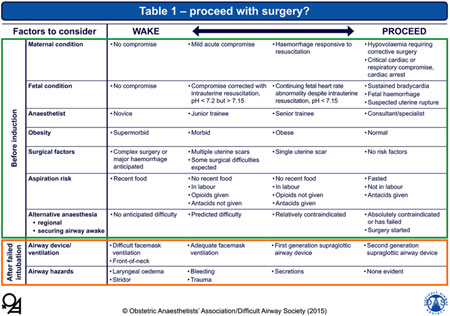 |
| |
Wake or proceed with surgery? Criteria to be used in the decision to wake or proceed following failed tracheal intubation. In any individual patient, some factors may suggest waking and others proceeding. The final decision will depend on the anaesthetist's clinical judgement. |
| |
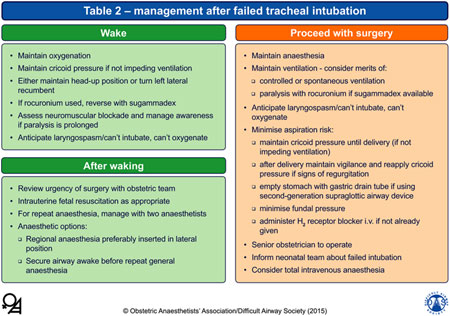
6. Table 2 – management after failed tracheal intubation: |
| |
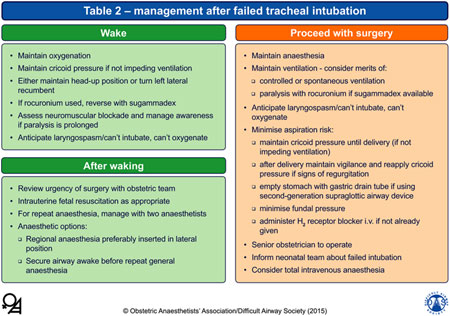 |
| |
Pre-theatre preparation |
| |
Airway assessment: |
| |
Every woman undergoing obstetric surgery should have an airway assessment to predict possible difficulty not only with tracheal intubation but also with mask ventilation or SAD insertion and front-of-neck access. |
| |
Factors that predict problems with tracheal intubation, mask ventilation, insertion of a supraglottic airway device and front-of-neck airway access. |
| |
|
Tracheal intubation |
Facemask ventilation |
SAD insertion |
Front-of-neck airway access |
| Body mass index > 35 kg.m−2 |
x |
x |
x |
x |
| Neck circumference > 50 cm |
x |
x |
x |
x |
| Thyromental distance < 6 cm |
x |
x |
x |
|
| Cricoid pressure |
x |
x |
x |
|
| Mallampati grade 3–4 |
x |
x |
|
|
| Fixed cervical spine flexion deformity |
x |
|
|
x |
| Dentition problems (poor dentition, buck teeth) |
x |
|
x |
|
| Miscellaneous factors (obstructive sleep apnoea, reduced lower jaw protrusion, airway oedema) |
x |
x |
|
| |
| Mouth opening < 4 cm |
x |
|
|
|
|
| |
Fasting status and antacid prophylaxis: |
| |
Gastric clearance in the pregnant woman who is not in labour is the same as in the non-pregnant patient. Labour and opioid analgesia delay gastric emptying, especially of food, but it returns to normal by 18 h post-delivery. |
| |
Current guidance for elective non-obstetric surgery suggests that food should be withheld for 6 h, whereas clear fluids may be given up to 2 h pre-operatively. |
| |
The commonest regimen for stomach preparation before elective caesarean section is a combination of a H2-receptor antagonist the night before and two hours before anaesthesia, with or without a prokinetic drug. If general anaesthesia is being used, sodium citrate is also administered immediately before induction. |
| |
Low-risk women are allowed a light diet. High-risk women should not eat but may have clear oral fluids, preferably isotonic drinks, together with oral administration of H2-receptor antagonists every 6 h. |
| |
If anaesthesia is required for delivery, an H2-receptor antagonist should be given intravenously if not already administered, with the aim of reducing the risk of aspiration at extubation. Sodium citrate should be given as for elective cases. |
| |
Wake or proceed with surgery? |
| |
Before induction of anaesthesia, the anaesthetist should discuss with the obstetric team whether to wake the woman or continue anaesthesia in the event of failed tracheal intubation. This decision is influenced by factors relating to the woman, fetus, staff and clinical situation, most of which are present pre-operatively (Table 1). |
| |
Fetal compromise is a more common indication for urgent caesarean section than maternal compromise. Although maternal safety is a greater priority for the anaesthetist than fetal, women willingly accept some risk to themselves to ensure a good neonatal outcome. |
| |
The overriding indications to proceed with general anaesthesia are maternal compromise not responsive to resuscitation, and acute fetal compromise secondary to an irreversible cause. |
| |
The firm indications to wake the mother up are periglottic airway swelling and continuing airway obstruction in the presence of optimised SAD or facemask management. |
| |
Rapid sequence induction: |
| |
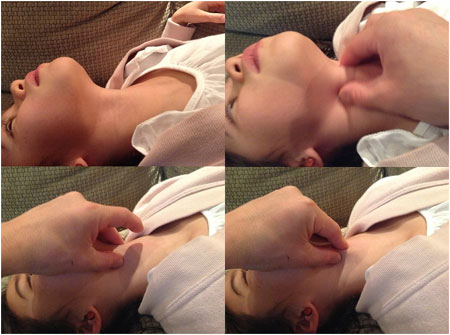
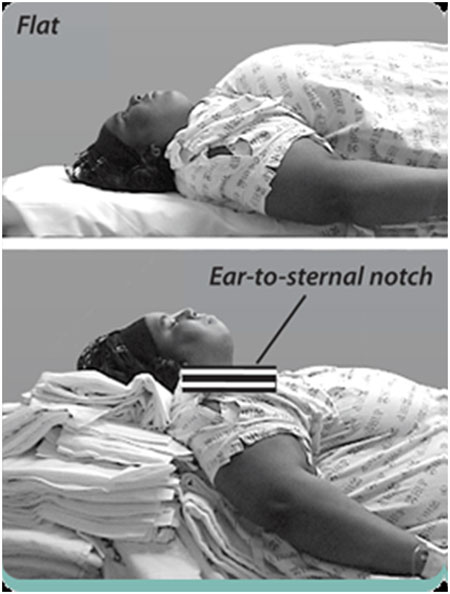
Optimise patient position |
| |
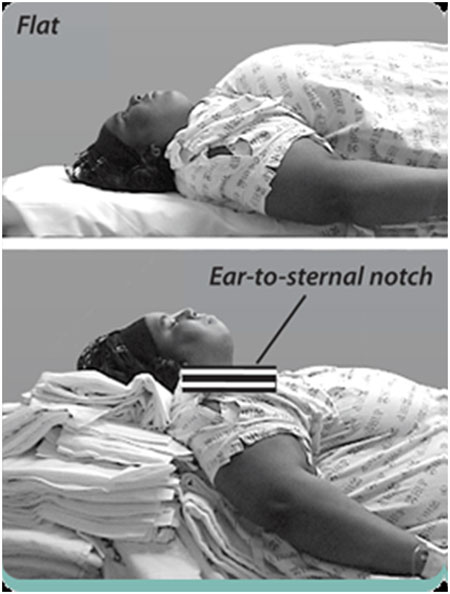
Optimal positioning is essential before the first intubation attempt. In addition to lateral uterine displacement as indicated, the head-up position should be considered. A 20–30o head-up position increases functional residual capacity in pregnant women and safe apnoea time in non-pregnant obese and non-obese patients. It also decreases difficulty with insertion of the laryngoscope caused by large breasts, improves the view at laryngoscopy and may reduce gastro-oesophageal reflux. In the morbidly obese patient, the ‘ramped’ position, aligning the external auditory meatus with the supra-sternal notch, has been shown to be superior to the standard ‘sniffing position’ for direct laryngoscopy. |
| |
 |
| |
Pre-oxygenation |
| |
Pre-oxygenation increases the oxygen reserve in the lungs during apnoea. End-tidal oxygen fraction (FETO2) is the best marker of lung denitrogenation, an FETO2 ≥ 0.9 is recommended. |
| |
A fresh gas flow rate of ≥ 10 l.min−1 is required for effective denitrogenation, and a tight mask-to-face seal is essential to reduce air entrainment. |
| |
Most anaesthetists pre-oxygenate for ≥ 3 min even during category-1 caesarean section; however, previous clinical research and recent computer modelling shows that a 2-min period of pre-oxygenation is adequate for the term pregnant woman at term. |
| |
If the patient is apnoeic and the airway is not being instrumented, continued administration of 100% oxygen with a tightly fitting facemask and maintenance of a patent airway allows continued oxygenation by bulk flow to the alveoli (apnoeic oxygenation). The anaesthetist should consider attaching nasal cannulae with 5 l.min−1 oxygen flow before starting pre-oxygenation, to maintain bulk flow of oxygen during intubation attempts. |
| |
Cricoid pressure |
| |
Current evidence supports applying 10 N force initially and then increasing to 30 N after loss of consciousness, as too much force (e.g. 44 N) is associated with airway obstruction. If the head-up position is used for induction, this force can be reduced to 20 N. It should be removed for insertion of a SAD. |
| |
Deliver appropriate doses of induction agent/neuromuscular blocking drug |
| |
There are strong recommendations to use Propofol instead of Thiopentone which suppresses airway reflexes more effectively and it may be an advantage if intubation fails. |
| |
Suxamethonium has been the standard neuromuscular blocking drug for rapid sequence induction as it had a faster onset and shorter duration than the alternatives. A unique disadvantage is that suxamethonium increases oxygen consumption through its depolarising action, and hence may cause earlier desaturation than rocuronium. |
| |
The use of high-dose rocuronium (1.0–1.2 mg.kg−1) with sugammadex backup is a suitable alternative to suxamethonium, as rocuronium can be fully reversed by sugammadex (16 mg.kg−1) within 3 min compared with 9 min for the spontaneous offset of suxamethonium. |
| |
Consider facemask ventilation |
| |
Currently, gentle bag/facemask ventilation (maximal inflation pressure < 20 cmH2O) is recommended after administration of induction drugs during rapid sequence induction as it can reduce oxygen desaturation and may allow an estimation of the likelihood of successful bag–facemask ventilation should it be required during prolonged or failed intubation attempts. |
| |
First intubation attempt |
| |
A short-handled Macintosh laryngoscope has been the device of choice with McCoy blades and obtuse angle devices (e.g. polio blade). |
| |
Videolaryngoscopes usually provide a better view of the glottis than direct laryngoscopes. |
| |
If a poor view of the larynx is obtained at the first laryngoscopy, attempts should be made to improve the view by reducing or removing cricoid pressure, external laryngeal manipulation and repositioning the head and neck. Insertion of the tracheal tube can be facilitated with the use of a tracheal tube introducer (bougie) or a stylet. Small tracheal tubes (e.g. size 7.0) should be used routinely to improve the success rate and minimise trauma. |
| |
Second intubation attempt |
| |
If the first attempt at intubation fails, the second attempt should be by the most experienced anaesthetist present, using alternative equipment as appropriate. If delay is anticipated, we recommend that mask ventilation is recommenced during preparation. Cricoid pressure should be released as it may be the cause of the poor view; however, the view of the larynx may be improved by external laryngeal manipulation guided by the anaesthetist. |
| |
If there is a grade-3b or -4 view at laryngoscopy, the success rate of blind insertion of a bougie or tracheal tube is low and the risk of airway trauma is high. |
| |
A third attempt at intubation should only be by an experienced anaesthetist. Administration of a further dose of intravenous anaesthetic should be considered to prevent awareness. |
| |
Verify tracheal intubation |
| |
A sustained capnographic trace is the most reliable method of confirming tracheal intubation. |
| |
Algorithm 2 – obstetric failed tracheal intubation: |
| |
If the second intubation attempt is unsuccessful, a failed intubation must be declared to the theatre team who should call for further help from an experienced anaesthetist. Once a failed intubation has been declared, the focus is to maintain oxygenation via either a facemask or a SAD, and prevent aspiration and awareness. An oropharyngeal airway, a four-handed (two-person) technique and release of cricoid pressure should be used if facemask ventilation is difficult. |
| |
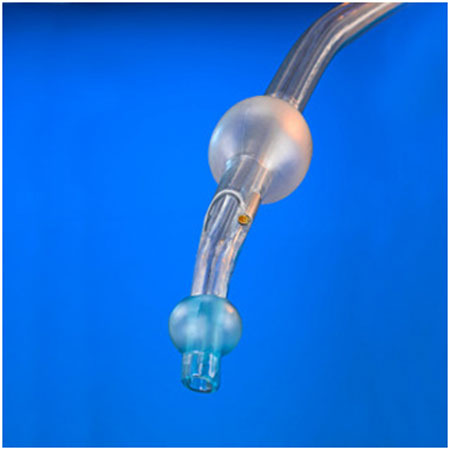
Immediate insertion of a SAD is the preferred choice before the induction agent and suxamethonium wear off. Use of a laryngoscope may aid SAD placement. We recommend that cricoid pressure should be released temporarily during insertion of a SAD. A second-generation SAD with a gastric drain tube is recommended to allow the passage of a gastric tube and the ability to generate higher inflation pressures. We recommend a maximum of only two insertion attempts. |
| |
Algorithm 3 – ‘can't intubate, can't oxygenate’ |
| |
When a ‘can't intubate, can't oxygenate’ situation has been declared, specialist help such as ear, nose and throat surgeon and/or intensivist should be called. |
| |
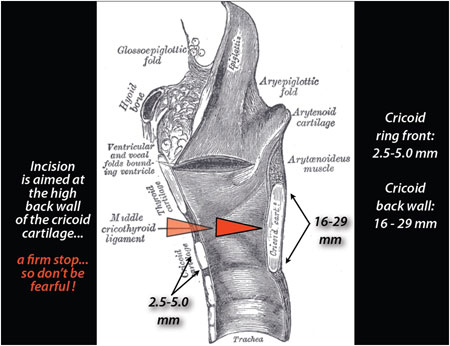
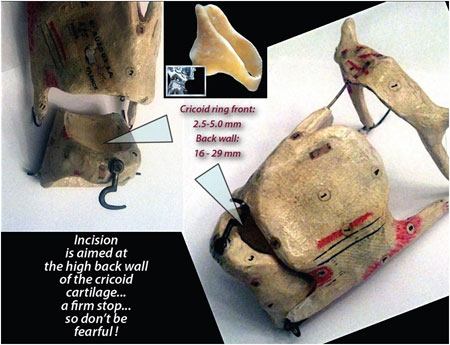
Front-of-neck procedure |
| |
If the front-of-neck procedure fails to restore oxygenation, a cardiac arrest protocol should be instituted, including caesarean delivery if there is an undelivered fetus of > 20 weeks' gestation. |
| |
 |
| |
Is it safe or essential to proceed with surgery immediately? |
| |
If adequate oxygenation is achieved by any method after failed intubation, the provisional decision to wake the patient or continue general anaesthesia and proceed with surgery should be reviewed, especially with regard to a possible change in severity of maternal or fetal compromise. |
| |
Management after failed tracheal intubation |
| |
Wake |
| |
If the decision is made to wake the patient following a failed intubation, oxygenation needs to be maintained while avoiding regurgitation and the recent guidelines usually suggest maintaining the supine position with lateral uterine displacement. |
| |
Following waking, the urgency of delivery should be reviewed with the obstetrician. The preferred options are regional anaesthesia or securing the airway while awake followed by general anaesthesia. |
| |
Proceed with surgery |
| |
When the decision has been made to continue with general anaesthesia and surgery, key issues to consider are: choice of airway device and ventilation strategy; maintenance of anaesthesia; use of cricoid pressure; drainage of gastric contents; and plans to perform delayed tracheal intubation if required. |
| |
A decision to use spontaneous or controlled ventilation should be made on a case-by-case basis. |
| |
Source: |
| |
Obstetric Anaesthetists' Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics.
|
| |
Anaesthesia: Volume 70, Issue 11, pages 1286–1306, November 2015.
|