| ANAESTHESIA PEARLS |
| A good anaesthetist should keep following points in mind at the time of laparoscopic surgery | |||||||||||||||||||||||||||||||
|
 |
||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
| Anaesthesia for laparoscopic surgery - Paul Hayden and Sarah Cowman | |||||||||||||||||||||||||||||||
| Anesthesia for Laparoscopic Surgery - John H. Nguyen, MD, Pedro P. Tanaka, MD, PhD | |||||||||||||||||||||||||||||||
| Anesthetic Implications of Laparoscopic Surgery Anthony J. Cunningham | |||||||||||||||||||||||||||||||
-
Local anesthetic systemic toxicity (LAST)
 |
Estimated incidence of 4 per 10000.Lipid emulsion has emerged as a possible antidote for systemic toxicity. ASRA and AAGBI recommend the same dosing for 20% lipid emulsion; A 1.5 mL/kg bolus administered over 1 min followed by A continuous infusion of 0.25 mL/kg/min until 10 min after hemodynamic stability is obtained Two additional boluses may be administered in the absence of a response to the first bolus, and the infusion rate may be increased to 0.5 mL/kg/min if there is persistent hypotension. Approximately 10 mL/kg lipid emulsion for 30 mins is recommended as an upper limit for initial administration. | |||||||||||||||||||||||||||||||||||
The American Society of Regional Anesthesia and Pain Medicine (ASRA) expert panels recommendations for the prevention, diagnosis, and treatment of LAST. |
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Pearls from the article include: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Pre-oxygenation extends the duration of safe apnoea in emergency tracheal intubation | ||
| Patients with normal respiratory drive should be pre-oxygenated for 3 minutes or take 8 maximal inhalation/exhalation breaths | ||
| NIV (non-invasive ventilation) should be considered for pre-oxygenation and ventilation during the onset phase of muscle relaxation in patients who cannot achieve saturations greater than 93-95 % with high FiO2 | ||
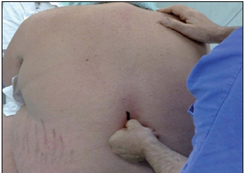
| Patients should be positioned in the head up position whenever possible. In patients with spinal precautions, reverse trendelenburg can be used | ||
| Apnoeic oxygenation can extend the duration of safe apnoea when used with sedation and muscle relaxants. A nasal cannula set at 15L/min is an effective means of providing this during ED intubations. | ||
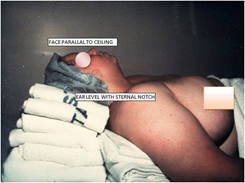
| For intubation, patients should be positioned to maximize upper airway patency before and during the apnoeic period, using ear to sternal positioning. Nasal airways and jaw thrust may help to create a patent airway. | ||
| In patients at high risk of desaturation, rocuronium may provide a longer duration of safe apnoea than succinylcholine. |
| You may not be familiar with one technique that we mention below, so-called “DSI” or Delayed Sequence Intubation. | ||
| Standard RSI consists of the simultaneous administration of a sedative and a paralytic agent and the provision of no ventilations until after endotracheal intubation. This sequence can be broken to allow for adequate preoxygenation without risking gastric insufflation or aspiration; we call this method “delayed sequence intubation” (DSI). | ||
| Managing difficult airways in obese patients. The best part is the simple mnemonic that makes it so easy to remember. | ||
|
 |
![]() AIRWAY CORRECTION
AIRWAY CORRECTION
 | |||
Ref: | |||
| THE MNEMONIC: Remember with obese patients, build a BIG RAMPPPP | |||
|
B: BUY TIME: Increase FiO2, NIV, Optimise Medical Rx
I: INDICATION FOR INTUBATION: do you really need to do it & do it now?
G: GET HELP: Anaesthetics, ICU, ENT, Nurses, Orderlies
R: RAMP: Build a big ramp!
A: APNOEIC OXYGENATION: use nasal prongs to maintain diffusion of O2
M: MINIMAL DRUGS: local anaesthetic spray/neb, ketamine/ketofol +/- sux/roc
P: PRE-OXYGENATE WITH NIV
P: PARALYSIS – ONLY IF NEEDED
P: PLAN FOR FAILURE: Surgical airway kit by the bedside
P: POST INTUBATION CARE
| |||
Ref: | |||