| ANAESTHESIA PEARLS |
| Crisis Management during Anaesthesia | |||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
| All anaesthetists have to handle life threatening crises with little or no warning. However, some cognitive strategies and work practices that are appropriate for speed and efficiency under normal circumstances may become maladaptive in a crisis. So, they have designed a Crisis Management Manual which can be adapted in all crisis situations. | |||||||||||||||||||||||||||||||||||||||||||||
| The ‘‘core’’ algorithm (based on the mnemonic COVER ABCD–A SWIFT CHECK) would diagnose and correct the problem in 60% of cases and provide a functional diagnosis in virtually all of the remaining 40%. For managing the problems underlying the remaining 40% of crises 24 specific Sub-algorithms were therefore developed. | |||||||||||||||||||||||||||||||||||||||||||||
| COVER should be applied into four levels represented by the mnemonic ‘‘SCARE’’, depending on the degree of perceived urgency (Scan-Check-Alert/Ready-Emergency). | |||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
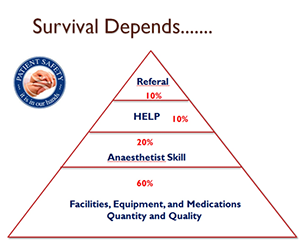
| In Crisis Management the Patient Survival Depends.......... | ||||||||||||||||||||||||||||||||||||||||||||
| The safe practice of Anaesthesia starts with the patient. A well pre-operatively optimized patient, the availability of modern facilities, equipments and medication in good quality and quantity at time of crisis and the skill of the attending Anaesthetist are all collectively determines the final outcome of the crisis. So the patient safety is in our hand. | ||||||||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||||||||
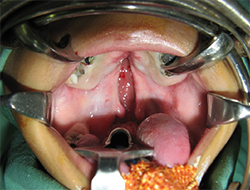
| Cleft Palate – Remember 5 points | ||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
| Approach | ||||||||||||||||||||||||||||||||||||||||||||
| Intraoral route - The nerve is accessed through the sub-sulcal area in the buccal mucosa at the junction of premolars 1 and 2. | ||||||||||||||||||||||||||||||||||||||||||||
| Palpate infraorbital foramen with index finger and use to guide needle and retract the cheek with the thumb. Insert the needle into the mucobuccal fold at junction of premolars 1 and 2. Direct the needle parallel to the long axis of premolar 2, palpating its location as the needle is advanced until it is adjacent to the infraorbital foramen. 0.5 to 1ml of local is usually enough. | ||||||||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||||||||
For neonates anatomy is different: Halfway between the midpoint of palpebral fissure and the angle of the mouth. Bosenberg. BJA 1995; 74: 506-508. |
||||||||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||||||||
Dose: For infants scheduled for cleft lip repairs, use 0.5mL of local anesthetic solution for each side, for older children and adolescents; use 1.5 mL to 2 mL of local anesthetic solution. |
||||||||||||||||||||||||||||||||||||||||||||
| Ref: | ||||||||||||||||||||||||||||||||||||||||||||
| 1. Peripheral Nerve Blocks For Children; NYSORA. | ||||||||||||||||||||||||||||||||||||||||||||
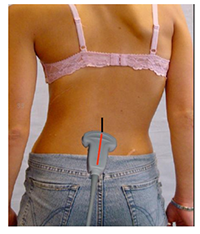
Ultrasound for Epidurals… |
||||||||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||||||||
Ultrasound has recently been utilized to facilitate lumbar spinals and epidurals. Spinal ultrasound is especially challenging, because the structures we need to image are protected by a very complex, articulated encasement of bones, which affords very limited acoustic windows for the ultrasound beam. In addition, the structures we want to visualize are located even deeper than we are accustomed to when we use ultrasound for peripheral nerve blocks or central lines. For these reasons, the ultrasound probe used for spinals and epidurals must be a low frequency, curved probe (2-5 mHz). The low frequency ultrasound beam penetrates deeper, but loses in image resolution. |
||||||||||||||||||||||||||||||||||||||||||||
There are two acoustic windows that are effective for lumbar spine sonographic assessment: one seen on the transverse approach, and the other seen on the longitudinal paramedian approach. The information from each of these two scanning planes supplements the other.3 |
||||||||||||||||||||||||||||||||||||||||||||
Despite widespread enthusiasm for using lumbar ultrasound in obstetrics, there are some who believe it is expensive and time-consuming, with undetermined risks and uncertain benefits. |
||||||||||||||||||||||||||||||||||||||||||||
| Indeed, obstetric anesthesiologists have managed to do this with great success without using imaging techniques. There is a long learning curve associated with lumbar ultrasound and it is unclear from the literature if the success rates associated with its use are superior to clinical skill alone6. | ||||||||||||||||||||||||||||||||||||||||||||
| Ref: | ||||||||||||||||||||||||||||||||||||||||||||
| 1. Chris’s tips in beautifully illustrated form of Ultra sound for Epidurals | ||||||||||||||||||||||||||||||||||||||||||||
2. Ultrasound for the Guidance of Epidural Analgesia, Anaesthesiologynews.com |
||||||||||||||||||||||||||||||||||||||||||||
3. Ultrasound-Facilitated Epidurals and Spinals in Obstetrics. |
||||||||||||||||||||||||||||||||||||||||||||
6. Lumbar ultrasound: useful gadget or time-consuming gimmick? |
||||||||||||||||||||||||||||||||||||||||||||
| Postoperative Airway Complications after Cleft Palate Repair | ||||||||||||||||||||||||||||||||||||||||||||
 |
||||||||||||||||||||||||||||||||||||||||||||
Airway complications after Cleft Palate repair range from episodes of mild stridor (noisy, snoring-like breathing resulting from obstruction in the naso- or oropharynx) to complete loss of the airway requiring re-intubation. |
||||||||||||||||||||||||||||||||||||||||||||
Anaesthetic or surgical complications: |
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
Perioperative Strategies to Minimise Airway Complications after Palate Surgery |
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
Nasopharyngeal Airway Size |
||||||||||||||||||||||||||||||||||||||||||||
Diameter |
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
Length |
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
| Ref: | ||||||||||||||||||||||||||||||||||||||||||||
Postoperative Airway Complications after Cleft Palate Repair, Anaesthesia Tutorial of the Week – 237 |
||||||||||||||||||||||||||||||||||||||||||||
Guidelines for insertion of Nasopharyngeal airway (NPA) |
||||||||||||||||||||||||||||||||||||||||||||
| Ref: | ||||||||||||||||||||||||||||||||||||||||||||
Great Ormond Street guidelines on preparation and management of nasopharyngeal airways |
||||||||||||||||||||||||||||||||||||||||||||