| |
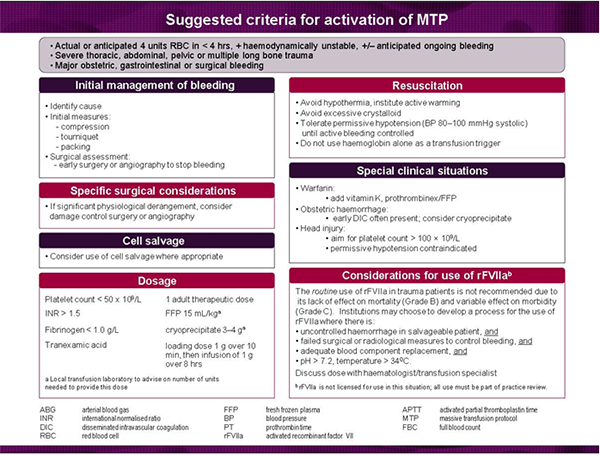
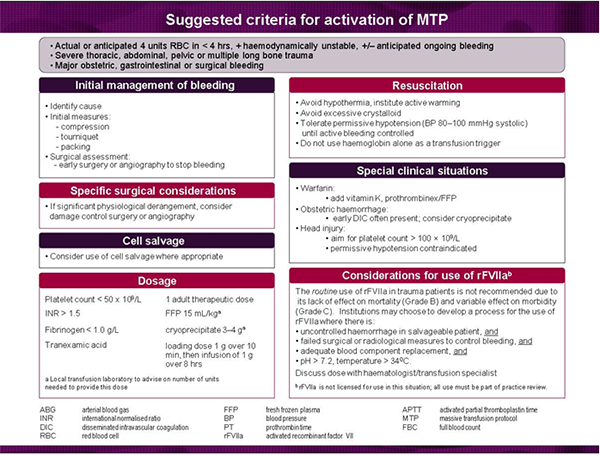
MASSIVE HAEMORRHAGE TREATMENT (MTP) PROTOCAL |
| |
|
|
| |
Casey Parker |
| |
 |
| |
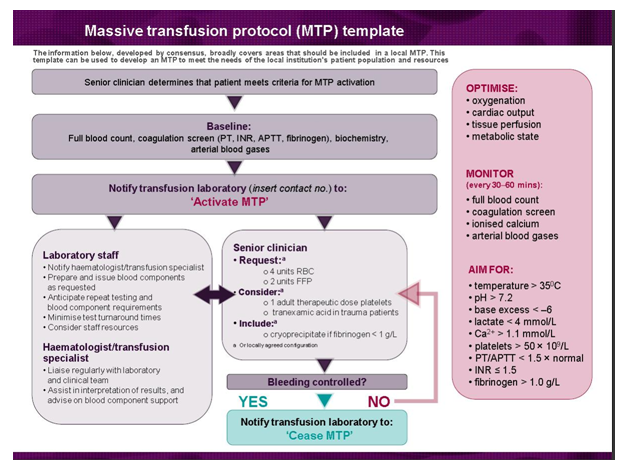
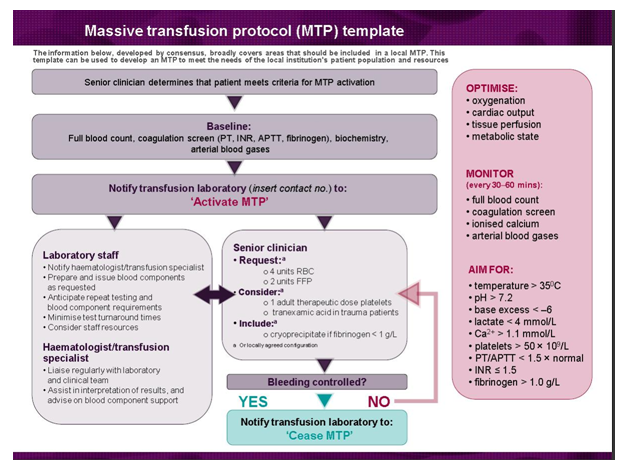
An example of a Major Haemorrhage Protocol
(If there is local Protocol for your Hospital that should be used) |
| |
Definition |
| |
Massive transfusion is arbitrarily defined as the replacement of a patient's total blood volume in less than 24 hours, or as the acute administration of more than half the patient's estimated blood volume per hour. |
| |
STEP 1: Bleeding control |
| |
|
| |
STEP 2: Identify the need for Massive Transfusion |
| |
A: Use a clinical prediction rule to stratify the need for MTP: |
| |
Assessment Scores: |
| |
|
| |
B: Identify massive trauma / bleed on purely clinical basis – “the Crashing Patient” |
| |
| |
 |
Poly trauma with multiple system injuries and unstable haemodynamics. |
| |
 |
Massive post-partum haemorrhage with measured blood loss > 1500 mls. |
| |
 |
Post-surgical bleeding from major vessels. |
| |
 |
GI bleeding with shock. |
|
| |
STEP 3: Activate Hospital Massive Transfusion system |
| |
| |
 |
Lab team need to know early – they will need to prep products and process your incoming blood samples.
|
| |
 |
Early thawing of 2 units FFP if large volumes are expected. |
| |
 |
Dedicated nurse / team member to run the rapid infusion device. |
| |
 |
Orderly to run samples and bloods to the lab for processing. |
| |
 |
Scribe to document the products / volumes and response. |
|
| |
STEP 4: Initial Empirical Resuscitation (first 15 – 30 minutes) |
| |
Take bloods for URGENT processing: |
| |
FBP, cross match, coagulation profile (INR, APTT, fibrinogen), ABG (VBG) |
| |
|
| |
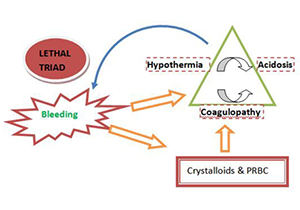
Remember the following Lethal Triad |
| |
|
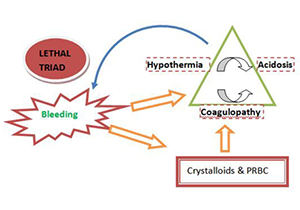 |
| |
STEP 5: Continue Volume Resuscitation / Monitoring |
| |
|
A: Continue PRBCs and FFP in 1:1 ratio – target MAP is 65 – 70 mmHg |
| |
|
|
NB: target MAP is 90 – 100 in patients with traumatic brain injury / raised ICP suspected |
| |
|
B : Monitoring – establish early and use to titrate specific agents / interventions |
| |
|
|
| |
 |
Recommend invasive monitoring (arterial line) if available. |
| |
 |
Send repeat investigations every ~ 30 minutes: FBP, coagulation profile, fibrinogen, ABG / lactate, Ca++. |
| |
 |
Frequent / continuous temperature monitoring. |
|
| |
STEP 6: Consider other agents for prevention / limitation of coagulopathy |
| |
|
| |
 |
Warfarinised / known coagulopathy : give Vit K 10 mg, Human Prothrombin Complex (Prothrombinex) (25 iu/kg = ~ 4 vials for 80 kg pt) |
| |
 |
Obstetric haemorrhage: early use of cryoprecipitate is recommended. |
| |
 |
Platelets: only recommended in thrombocytopenia < 50,000. |
| |
 |
Tranexamic acid: give 1 g loading dose (over 10 mins) as early as possible in traumatic bleeding. |
|
| |
STEP 7: Target therapy to results / Clinical parameters |
| |
|
| Target therapy to results |
|
Clinical parameters |
 |
Target BP - MAP = 65 mmHg |
|
 |
Give fluid volume: ideally RBCs / FFP |
 |
IF Hb < 80 g/l |
|
 |
THEN Give RBCs |
 |
If INR > 1.5 OR APPT > 50 sec |
|
 |
Give 2u FFP consider Prothrombinex |
 |
If fibrinogen < 1.0g/l |
|
 |
Give 8 units of cryoprecipitate |
 |
If ion. Calcium is < 1.1 mmol |
|
 |
Give 1 amp of Ca-gluc 1g/10mls |
 |
Optimise acidosis |
|
 |
Consider intubation / ventilation => normocapnea |
 |
Maintain patient T > 35 deg |
|
 |
IV fluid warmer, Air blanket, limit exposure & operation time |
|
| |
The use of Recomb: |
| |
Factor VII remains controversial – this should only be used in consultation with Haematologist and once other reversible causes of coagulopathy have been addressed / targets reached. |
| |
STEP 8: Evacuation planning |
| |
| |
 |
In smaller centres the early evacuation planning should commence as soon as the patient is received. |
| |
 |
In the absence of a definitive surgical service – evacuation should be expatiated to such a centre. |
| |
 |
The retrieval team should be made aware of the product availability and stock so they can plan to bring further agents for the ongoing resuscitation / transfer. |
| |
 |
Suggest early liaison with RFDS, receiving hospital ED / surgeon and clinical Haematologist. |
|
| |
Ref: |
| |
1. Source: BroomeDocs: Massive Transfusion Protocol (MTP) |
| |
2. Management of massive blood loss: a template guideline. Br. J. Anaesth. (2000) 85 (3): 487-491. |
| |
3. Blood transfusion and the anaesthetist: management of massive haemorrhage Anaesthesia. 2010 November; 65(11): 1153–1161 |
| |
4. Management of bleeding following major trauma: an updated European guideline Critical Care 2010, 14:R52 |
| |
5. Management of Obstetric Haemorrhage Anaesthesia UK |
| |
6. Management of Obstetric Haemorrhage Anaesthesia Tutorial of the Week – 257 |
| |
7. Haemostatic monitoring during postpartum haemorrhage and implications for management Br. J. Anaesth. (2012) 109(6): 851-863 |
| |
8. Massive Transfusion Protocol (MTP) for Hemorrhagic Shock ASA Committee on Blood Management |
| |
9. Massive Transfusion Protocols for Patients With Substantial Hemorrhage Transfus Med Rev. 2011 October; 25(4): 293–303. |
| |
10. Transfusion in major haemorrhage UK Blood Transfusion & Tissue Transplantation Services |
| |
|
| |
Critical Bleeding Massive Transfusion |
| |
 |
| |
 |
| |
Critical Bleeding/Massive Transfusion module: National Blood Authority of Australia. |
| |
|
| |
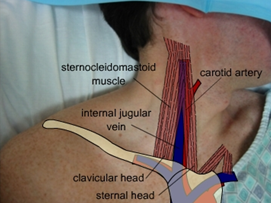
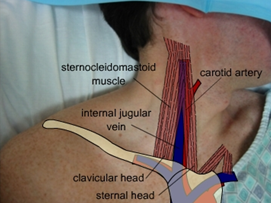
Central line in the Carotid..What to do ..Push..Pull..or Leave it |
| |
|
|
 |
| |
|
Percutaneous catheterization is a frequently-used technique to gain access to the central venous circulation. Inadvertent arterial puncture is often without consequence, but can lead to devastating complications if it goes unrecognized and a large-bore dilator or catheter is inserted. |
| |
|
Several studies have reported the incidence of arterial cannulation to be between 0.1-1.0%. |
| |
|
The most common injury to arteries is related to puncture or cannulation of the carotid artery. Puncturing the carotid artery with a small needle occurs in about 6% of all procedures and, although undesirable, does not generally produce any harm. However if the arterial puncture is not recognized and a guidewire is placed into the artery and followed with a CVC or a pulmonary artery catheter introducer sheath there is the possibility of a major problem. |
| |
|
Ultrasound and pressure waveform measurement are two commonly used methods to reduce the chances of injury to the carotid artery. |
| |
|
Several of the specific findings of the Guilbert et al. study are worth noting: |
| |
|
| |
 |
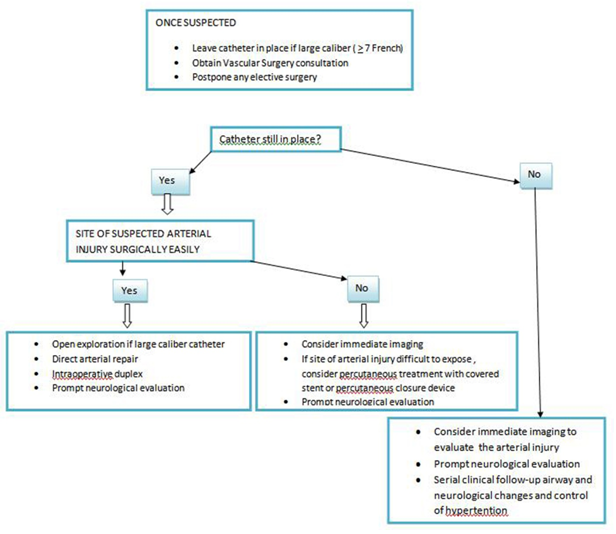
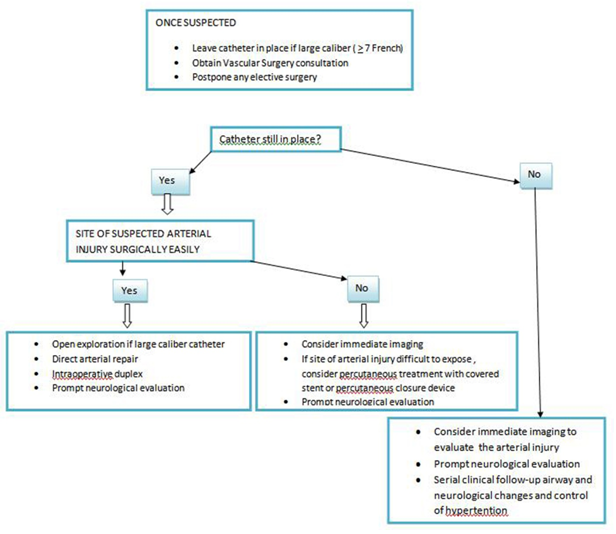
Arterial cannulation can occur despite the use of ultrasound guidance. |
| |
 |
The low internal jugular approach can injure the subclavian or innominate arteries or even the aorta.
Arterial injury below the sternoclavicular joint cannot be repaired through a cervical approach.
Clinical suspicion of an intrathoracic injury should prompt imaging to locate the site of injury and plan
surgical or endovascular treatment. |
| |
 |
Prolonged arterial cannulation can result in thrombus formation and stroke. |
| |
 |
A normal carotid duplex exam following removal of a catheter from the carotid does not rule out the
possibility of a stroke. Because of this, postponing elective surgery has been recommended to avoid
unrecognized stroke in an anesthetized patient. |
| |
 |
False aneurysms or arteriovenous fistulas can occur late following the pull/pressure technique, so
close follow-up is needed. |
|
| |
Proposed algorithm for cervical or thoracic arterial injury with a large-bore catheter |
| |
|
 |
| |
|
Source: JOURNAL OF VASCULAR SURGERY Volume 48, Number 4 |
| |
Ref: |
| |
|
1. Arterial trauma during central venous catheter insertion: Case series, review and proposed algorithm JOURNAL OF VASCULAR SURGERY Volume 48, Number 4 |
| |
|
2. Arterial Cannulation During Central Line Placement: Mechanisms of Injury, Prevention, and Treatment |
| |
|
3. Complication of central venous cannulation Can J Surg. 2008 October; 51(5): E113–E114. |
| |
|
4. Carotid Dissection: A Complication of Internal Jugular Vein Cannulation with the Use of Ultrasound A & A July 2009 vol. 109 no. 1 135-136 |
| |
|
| |
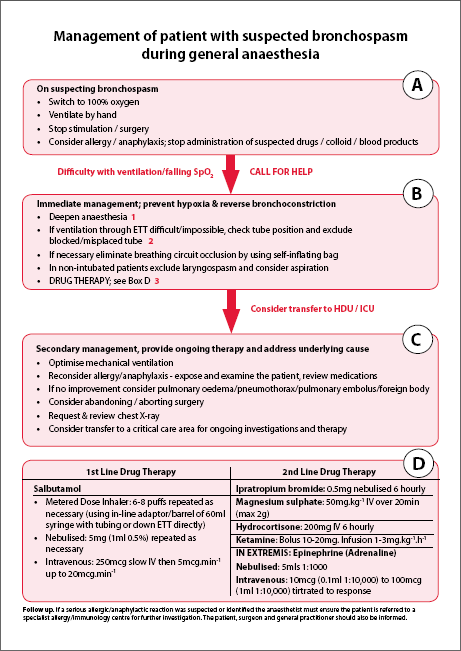
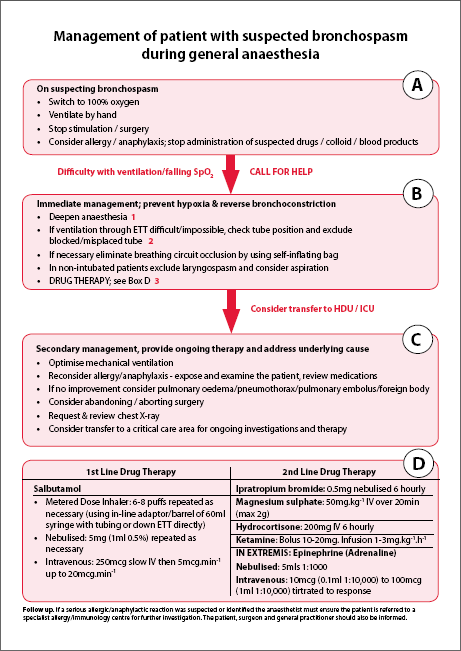
Management Of Patient With Suspected Bronchospasm |
| |
|
|
| |
|
 |
| |
|
Source |
| |
|
 Emergency algorithms,WFSA Education Resources Emergency algorithms,WFSA Education Resources |
|
|
| |
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation |
| |
CPR Overview |
| |
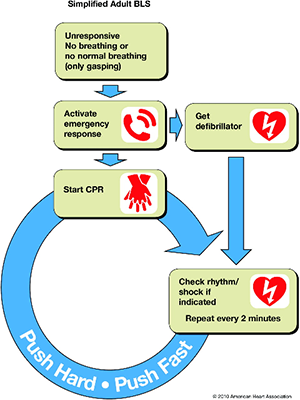
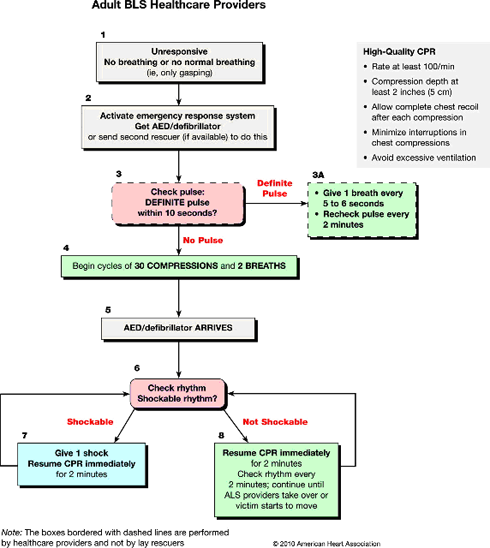
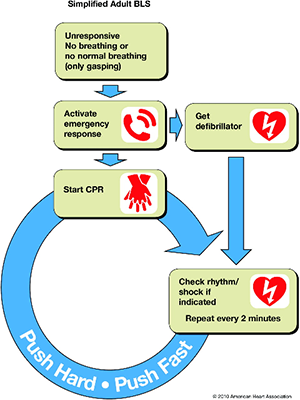
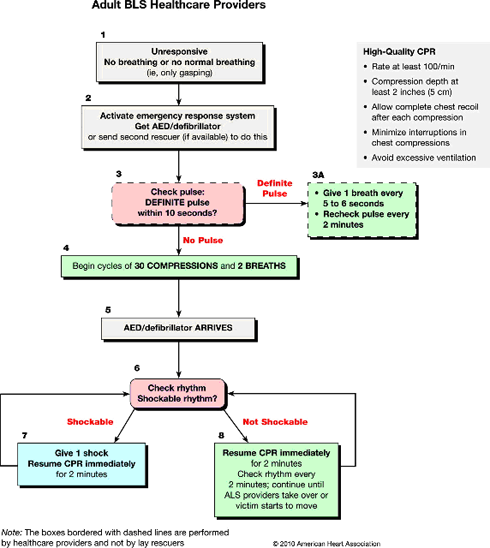
 Adult Basic Life Support Adult Basic Life Support
The major change made in BLS is a Change from A-B-C to C-A-B |
| |
Fundamental aspects of BLS include |
| |
 |
| |
|
| |
 |
Immediate recognition of sudden cardiac arrest (SCA) -
- No breathing, not breathing normally (eg, only gasping) |
 |
Activation of the emergency response system |
| |
|
 |
Early cardiopulmonary resuscitation (CPR), - Hands-Only CPR
Pulse Check - should take no more than 10 seconds
Chest Compressions - Compression depth of at least 2 inches/5
Allow complete recoil of the chest after each compression
A compression-ventilation ratio of 30:2
Rescue Breaths - Each rescue breath over 1 second
Sufficient to produce visible chest rise |
 |
Rapid defibrillation with an automated external defibrillator (AED). |
|
| |
 |
| |
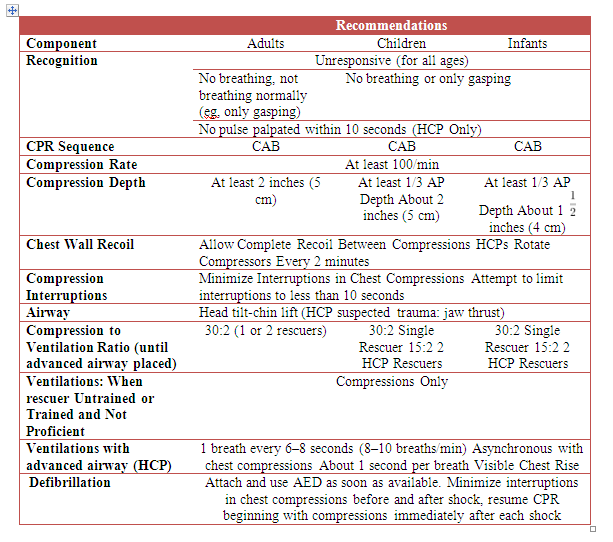
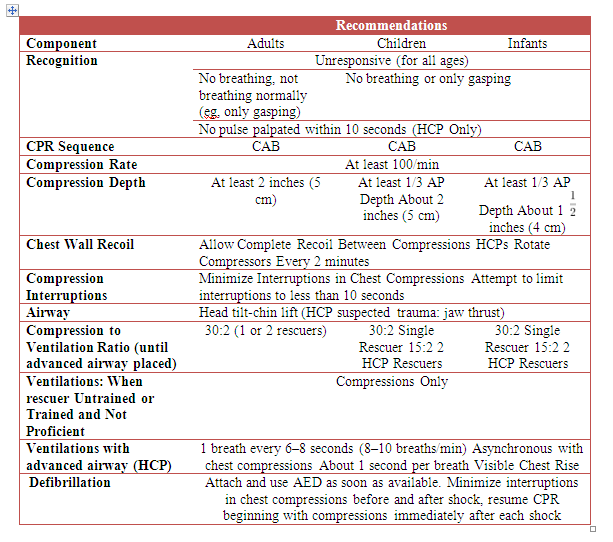
Continued Emphasis on High-Quality CPR: |
| |
The 2010 AHA Guidelines for CPR and ECC once again emphasize the need for high-quality CPR, including |
| |
 |
A compression rate of at least 100/min (a change from“approximately” 100/min)
|
 |
A compression depth of at least 2 inches (5 cm) in adults and a compression depth of at least one third of the anteroposterior diameter of the chest in infants and children(approximately 1.5 inches [4 cm] in infants and 2 inches[5 cm] in children). Note that the range of 1½ to 2 inches is no longer used for adults, and the absolute depth specified for children and infants is deeper than in previous versions the AHA Guidelines for CPR and ECC
|
 |
Allowing for complete chest recoil after each compression
|
 |
Minimizing interruptions in chest compressions
|
 |
Avoiding excessive(hyper) ventilation
|
|
| |
Adult BLS Skills: |
| |
The sequence of BLS skills for the healthcare provider is depicted in the BLS Healthcare Provider Algorithm |
| |
 |
| |
Summary of Key BLS Components for Adults, Children and Infants |
| |
 |
| |
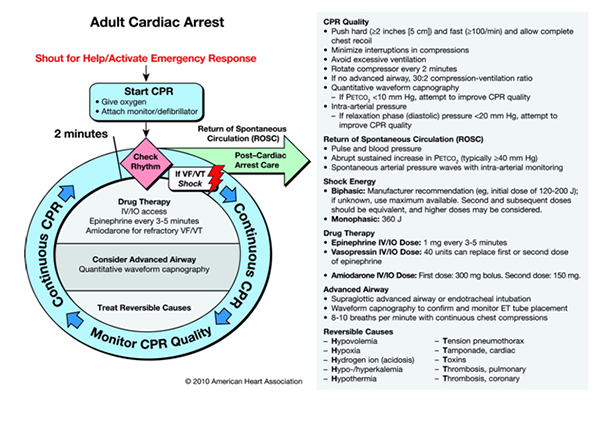
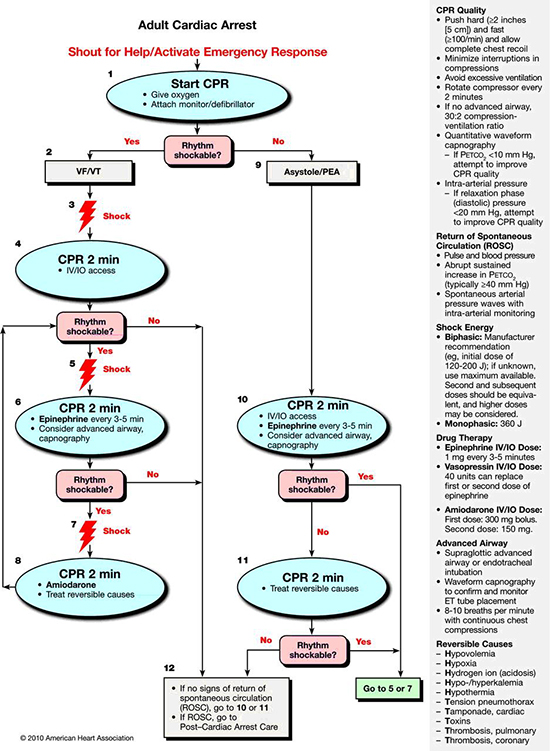
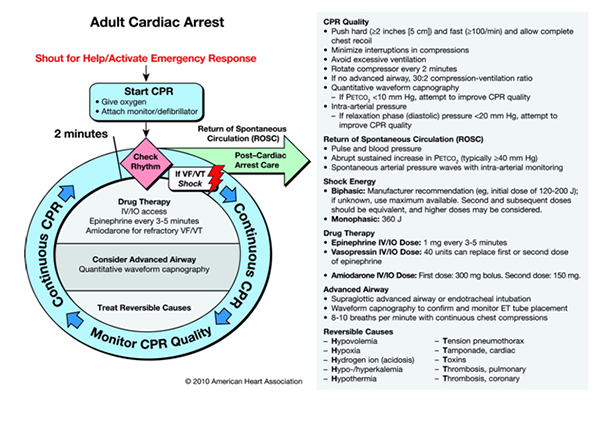
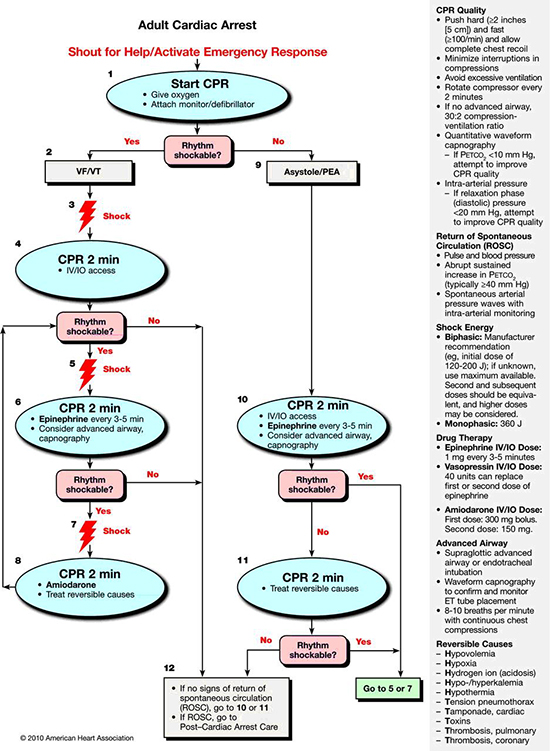
Adult Advanced Cardiovascular Life Support
|
| |
| Key changes from the 2005 ACLS Guidelines include: |
 |
Continuous quantitative waveform capnography is recommended for confirmation and monitoring of endotracheal tube placement.
|
 |
Cardiac arrest algorithms are simplified and redesigned to emphasize the importance of high-quality CPR.
|
 |
Atropine is no longer recommended for routine use in the management of pulseless electrical activity (PEA)/asystole.
|
 |
There is an increased emphasis on physiologic monitoring to optimize CPR quality and detect ROSC (Return of Spontaneous Circulation). Rhythm assessment using ECG and pulse checks as the only physiologic parameters to guide therapy. (Monitoring of Petco2, coronary perfusion pressure (CPP), and central venous oxygen saturation (Scvo2) provides valuable information on both the patient's condition and response to therapy).
|
 |
Chronotropic drugs (dopamine, epinephrine, and isoproterenol) infusions are recommended as an alternative to pacing in symptomatic and unstable bradycardia.
|
 |
Adenosine is recommended as a safe and potentially effective therapy in the initial management of stable undifferentiated regular monomorphic wide-complex tachycardia.
|
|
| |
The new circular algorithm is introduced in 2010 emphasizes the importance of high-quality CPR.
|
| |
 |
|
 |
| |
Ref: |
| |
|
1. Circulation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science |
| |
|
2. 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, Part 4: CPR Overview |
| |
|
3. 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, Part 5: Adult Basic Life Support |
| |
|
4. 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, Part 8: Adult Advanced Cardiovascular Life Support |
| |
|
| |
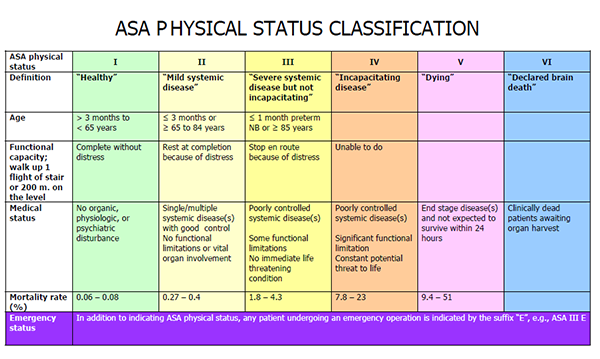
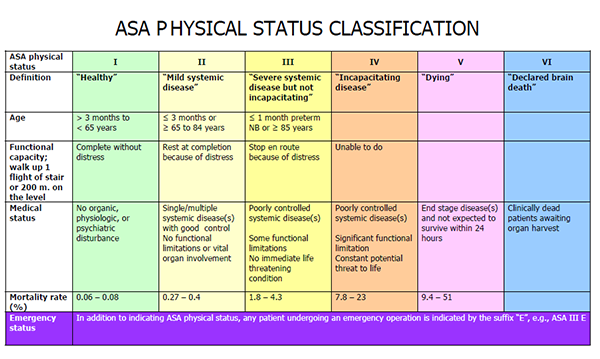
American Society of Anaesthesiologists physical status classification |
| |
 |
| |
 |
History |
|
| |
In 1940-41, ASA asked a committee of three physicians (Meyer Saklad, M.D., Emery Rovenstine, M.D., and Ivan Taylor, M.D.) to study, examine, experiment and devise a system for the collection and tabulation of statistical data in anesthesia which could be applicable under any circumstances. |
| |
They were given the task to devise a grading system to assess the operative risk, but after detailed studies research and discussion they stated that "In attempting to standardize and define what has heretofore been considered 'Operative Risk', it was found that the term ... could not be used. It was felt that for the purposes of the anesthesia record and for any future evaluation of anesthetic agents or surgical procedures, it would be best to classify and grade the patient in relation to his physical status only." |
| |
They described a six-point scale, ranging from a healthy patient (class 1) to one with an extreme systemic disorder that is an imminent threat to life (class 4). The first four points of their scale roughly correspond to today's ASA classes 1-4, which were first published in 1963.The original authors included two classes that encompassed emergencies which otherwise would have been coded in either the first two classes (class 5) or the second two (class 6). By the time of the 1963 publication of the present classification, two modifications were made. First, previous classes 5 and 6 were removed and a new class 5 was added for moribund patients not expected to survive 24 hours, with or without surgery. Second, separate classes for emergencies were eliminated in lieu of the "E" modifier of the other classes. |
| |
Original definition by Saklad et al. |
| |
| CLASS |
ORIGINAL |
| 1 |
No organic pathology or patients in whom the pathological process is localized and does not cause any systemic disturbance or abnormality. |
| 2 |
A moderate but definite systemic disturbance, caused either by the condition that is to be treated or surgical intervention or which is caused by other existing pathological processes, forms this group. |
| 3 |
Severe systemic disturbance from any cause or causes. It is not possible to state an absolute measure of severity, as this is a matter of clinical judgment. The following examples are given as suggestions to help demonstrate the difference between this class and Class 2. |
| 4 |
Extreme systemic disorders which have already become an eminent threat to life regardless of the type of treatment. Because of their duration or nature there has already been damage to the organism that is irreversible. This class is intended to include only patients that are in an extremely poor physical state. There may not be much occasion to use this classification, but it should serve a purpose in separating the patient in very poor condition from others. |
| 5 |
Emergencies that would otherwise be graded in Class 1 or Class 2. |
| 6 |
Emergencies that would otherwise be graded as Class 3 or Class 4. |
| |
|
|
| |
Source: Grading of Patients for Surgical Procedures Saklad, Meyer M.D. Anesthesiology: May 1941 - Volume 2 - Issue 3 - ppg 281-284 |
| |
In 1961, Dripps et all proposed a classification consists of 5 categories. |
| |
The new classification was amended by the 1962 House of Delegates of American Society of Anaesthesiologists,Inc. Two modifications were made in the new classification, the previous classes 5 and 6 were removed and a new class 5 was added for moribund patients not expected to survive 24 hours, with or without surgery. In addition emergency cases were designated by the letter 'E'. |
| |
The sixth class is a recent addition for declared brain dead organ donors. |
| |
A Physical Status (PS) Classification System |
| |
| ASA PS Category |
Preoperative Health Status |
| ASA PS 1 |
Normal healthy patient |
| ASA PS II |
Patients with mild systemic disease |
| ASA PS III |
Patients with severe systemic disease that limits activity, but is not incapacitating |
| ASA PS IV |
Patients with severe systemic disease that is a constant threat to life |
| ASA PS V |
Moribund patients who are not expected to survive 24 hours with or without the operation |
| ASA PS VI |
A declared brain-dead patient who organs are being removed for donor purposes |
| |
|
|
| |
E. Emergency surgery, E is placed after the Roman numeral. |
| |
The inconsistency and inadequacy of ASA grading system has been questioned for many years. The major drawbacks of this grading system are |
| |
 |
Inconsistency of grading between anesthetists. |
 |
Age; is not considered as an influencing factor, extremes of age like elderly patients and neonates may have poor tolerance to surgery and anaesthesia in the absence of systemic illness and cannot be considered as ASA 1 patients. |
 |
The grading system is not well suited for assessing physical status of special clinical conditions like burns, trauma and metabolic disorders. |
 |
No grade was available to describe moderate systemic illness. |
 |
The ASA Grading System shows poor inter rater reliability in pediatric practice. |
|
| |
Tomoaki and Yoshihisa reported that it is difficult to estimate whether the class II patients have an accurate risk ranging from mild to moderate-severe systemic disorders since the ASA class II is very broad and does not accurately reflect the patients’ risk. |
| |
They assessed 1933 patients scheduled for surgical procedures both by 5-grade ASA physical status protocol and by their new 7-grade preoperative status assessment dividing classes I and II into a and b. |
| |
SA Physical Status (7-grade) can provide a better grading outcome for predicting the incidence of intra- and postoperative complications in surgical patients. |
| |
| ASA Physical Status Classification |
Grade |
Revised classification |
| ASA PS 1 |
Ia |
Normal healthy patient. |
| |
Ib |
Patient with mild systemic disease.
Normal healthy patient with anaesthetic or operative risk. |
| ASA PS II |
IIa |
Patient with moderate systemic disease.
Patient with mild systemic disease with anaesthetic or operative risk. |
| |
IIb |
Patient with moderate to severe systemic disease that does not limit activity.
Patient with mild systemic disease with anaesthetic and operative risk.
Patient with moderate systemic disease with anaesthetic or operative risk. |
| ASA PS III |
|
Patients with severe systemic disease that limits activity, but is not incapacitating.
Patient with moderate systemic disease that does not limit activity with operative and anaesthetic risk(s)
Patient with moderate to severe systemic disease that does not limit activity with operative and anaesthetic risk(s) |
| ASA PS IV |
|
Patients with an incapacitating systemic disease that is a constant threat to life
Patients with severe systemic disease that limits activity, incapacitated |
| ASA PS V |
|
Moribund patients who are not expected to survive 24 hours with or without the operation |
| ASA PS VI |
|
A declared brain-dead patient who organs are being removed for donor purposes |
| |
|
|
|
| |
|
| |
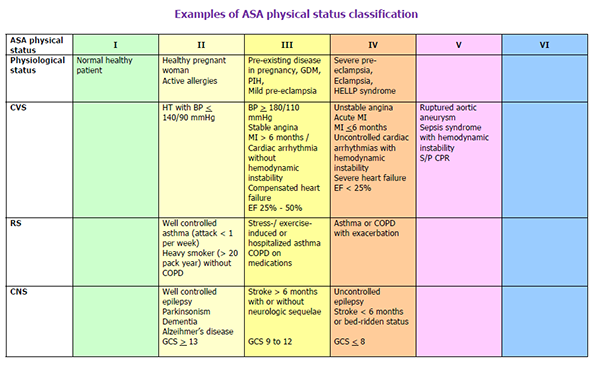
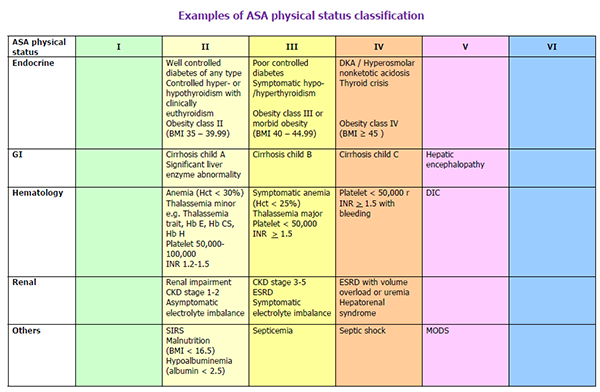
Examples of ASA physical status classification |
| |
|
| |
 |
| |
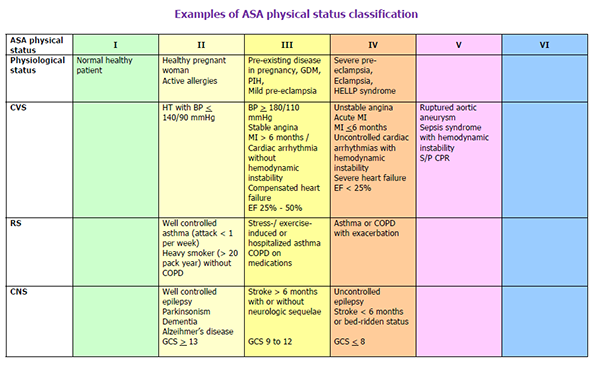 |
| |
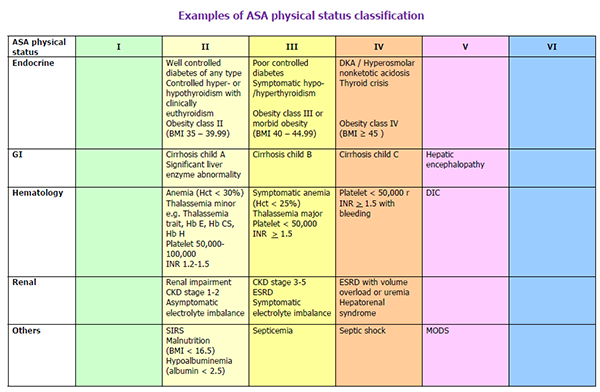 |
| |
Ref: |
| |
1. Grading of Patients for Surgical Procedures Saklad, Meyer M.D. |
| |
Anesthesiology: May 1941 - Volume 2 - Issue 3 - ppg 281-284 |
| |
2. Dripps RD Lamont A Eckenhoff JE : The role of Anaesthesia in surgical mortality. JAMA 178: 261-266, 1961 |
| |
3. New classification of physical status. Anesthesiology 1963; 24:111 |
| |
4. ASA Physical status Classification- A study of Consistency of Rating |
| |
Anaesthesiology 49:239-243,1978 |
| |
5. ASA Physical Status Classification System |
| |
6. American Society of Anaesthesiologists physical status classification |
| |
Indian J Anaesth. 2011 Mar-Apr; 55(2): 111–115. |
| |
7. Tomoaki H, Yoshihisa K. Modified ASA physical status (7 grades) may be more practical in recent use for preoperative risk assessment. |
| |
Internet J Anesthesiol. 2007;Vol. 15 |
| |
8. Asa revised 15102010 pdf : free ebook download from elearning |
| |
9. ASA physical status classification system From Wikipedia, the free encyclopedia |
| |
|
| |
|
|
|
|
 Adult Basic Life Support
Adult Basic Life Support