| |
Early Goal Directed Therapy in Septic Shock (EGDT) |
| |
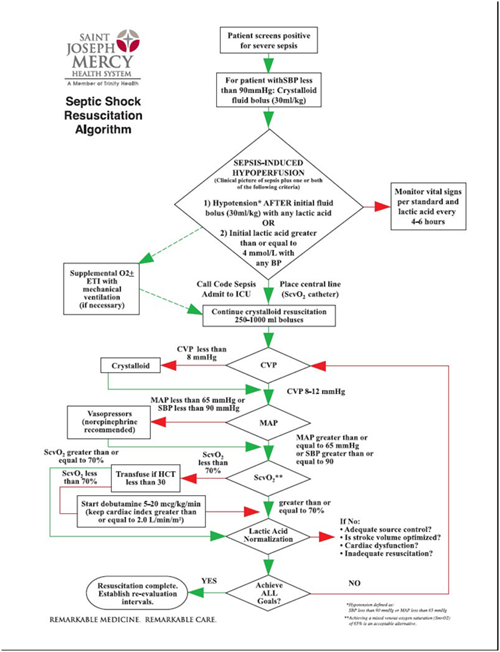
Early Goal Directed Therapy (EGDT) definition
|
| |
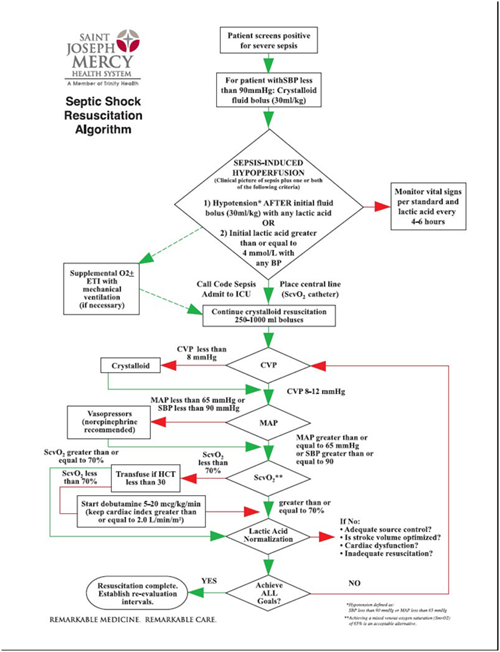
Within 6 hours of presentation to the Emergency Department intensive monitoring of specific circulatory parameters with the aggressive management of 5 key parameters to specified targets to optimise oxygen delivery to tissues. |
| |
Parameters |
| |
 |
CVP 8-12 mmHg |
 |
MAP 65 – 90 mmHg |
 |
Urine output >0.5 ml/kg/hr |
 |
Mixed venous oxygen saturation >65% / ScvO2 >70% |
 |
Haematocrit >30% |
|
| |
Interventions |
| |
 |
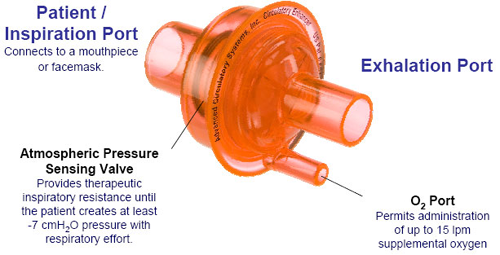
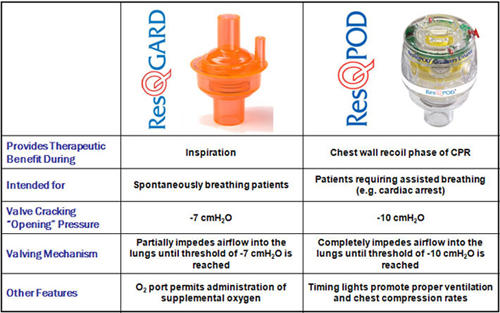
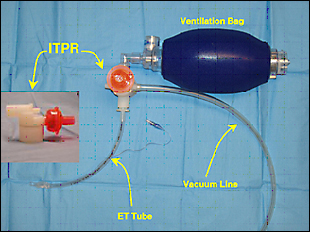
Reduce work of breathing by early use of mechanical ventilation |
 |
Fluid resuscitation |
 |
Use of vasoactive agents: noradrenaline, dobutamine |
 |
Transfusion |
|
| |
See the Rivers et al, 2001 EGDT protocol |
| |
Venous Oximetry – The concept of SvO2 and ScvO2 ! |
| |
| SvO2 >75% |
Normal extraction O2 supply > O2 demand |
| 75% > SvO2 > | 50% Compensatory extraction Increasing O2 demand or decreasing O2 supply |
| 50% > SvO2 > |
30% Exhaustion of extraction Beginning of lactic acidosis O2 supply < O2 demand |
| 30% > SvO2 > | 25% Severe lactic acidosis |
| SvO2 < 25% |
Cellular death |
• SvO2 - True mixed venous oxygen saturation
• ScvO2 - Central venous oxygen saturation
|
|
| |
 |
| |
RATIONALE |
| |
The rationale for EGDT is that early optimization of O2 delivery will improve outcome in sepsis |
| |
• Evidence supporting use found by the landmark Rivers Trial (NEJM, 2001) that showed a 16% mortality reduction when ScvO2 monitoring added to standard resuscitation target, although patients in treatment arm received more dobutamine and RBCs transfusion as well. |
| |
The principle of applying EGDT for septic shock is based on the observations that: |
| |
 |
Early treatment for Myocardial Infarction, Acute Ischaemic Stroke and Trauma improves patient outcomes |
 |
Patients presenting to ED with sepsis have measurable O2 deficit |
 |
O2 deficit is evidenced by high lactate and high ScvO2 |
 |
For septic shock the hypothesis is that early optimization of the compromised septic circulation may reduce mortality |
|
| |
 |
| |
ARGUMENTS FOR |
| |
 |
sensible end-point for O2 delivery as ScvO2 reflects supply-demand balance |
 |
our patients all have CVL in situ (in the ICU, not necessarily in the ED) |
 |
Rivers trial showed a substantial reduction in mortality with ScvO2 monitoring vs standard care |
 |
no other O2 delivery end point has been validated |
 |
recommended in Surviving Sepsis Guidelines |
 |
ScvO2 readily available |
 |
ScvO2 can have continuous monitoring |
 |
ScvO2 responds to therapy |
 |
ScvO2 is predictive of outcomes |
|
| |
ARGUMENTS AGAINST |
| |
Protocols for implementing EGDT usually result in more fluid being administered, more use of vasoactive medication and more use of blood transfusion which may lead to: |
| |
 |
Fluid overload (e.g. APO, abdominal compartment syndrome, edematous tissues impedding oxygen flux to cells) |
 |
Arrhythmias and myocardial necrosis from inotropes |
 |
Adverse effects of blood transfusion |
 |
Effects of excessive oxygen delivery |
|
| |
End-points (which parameter, and which value) are numerous and essentially arbitrary |
| |
 |
PCWP |
 |
CVP |
 |
systolic pulse pressure variation |
 |
pulse pressure variation |
 |
stroke volume variation |
 |
MAP |
 |
HR |
 |
SVRI |
 |
Q |
 |
SV |
 |
SpO2 |
 |
Hb/HCT |
 |
DO2 |
 |
GEDV |
 |
EVLW |
 |
ITLV |
 |
urine output |
 |
serum lactate |
|
| |
Endpoints based on cardiac output and other macrovascular parameters may not be very important |
| |
 |
macrovascular flow doesn’t mean microvascular flow |
 |
changes in sepsis (microvascular thrombi with endothelial dysfunction) |
 |
impaired autoregulation |
 |
microflow is linked to outcomes |
 |
microflow can be manipulated (dobutamine) |
|
| |
Proscriptive targets may not suit all (eg higher MAP needed for elderly patients, lower MAP and Hct targets for young, fit patients) |
| |
EVIDENCE |
| |
Limitations of Rivers study include the following: |
| |
 |
Study population limited to ED presentations and did not include ward patients |
 |
Single centre |
 |
Non-blinded |
 |
Control group had an above-average mortality rate and patients had high rates of comorbidities |
 |
‘Rivers effect’ (undivided attention of a critical care trained doctor in the intervention arm) |
 |
Unclear which interventions are most important – whole EGDT protocol or one single component |
 |
Target parameters are restrictive |
 |
Use of ScvO2 and pressure monitoring has not been tested in the target population |
 |
Transfusion target to improve DO2 contradicts restrictive transfusion practice and may be associated with increased mortality in the critically ill |
|
| |
Other approaches |
| |
 |
there is clear evidence from meta-analysis(Jones et al, 2008) that quantitative resuscitation within 24 hours, including approaches other than EGDT, improve mortality |
 |
targeting lactate clearance is non-inferior to EGDT Jones et al, 2010) |
|
| |
Results of Australasian ARISE and related international studies (US ProCESS and UK ProMISE) Awaited |
| |
AN APPROACH |
| |
 |
start early |
 |
optimize filling (dynamic tests of Starling curve: fluid responsiveness, swing) |
 |
best fluid controversial (not HES!) |
 |
optimise O2 carrying capacity |
 |
optimise oxygenation |
 |
optimize haemodynamics |
 |
augment contractility |
 |
can titrate to an end-point (ScvO2 or lactate) but it may not matter |
 |
await further higher quality evidence (e.g. ARISE, PROMISE and PROCESS) |
 |
We don’t use continuous ScVO2 monitoring |
|
| |
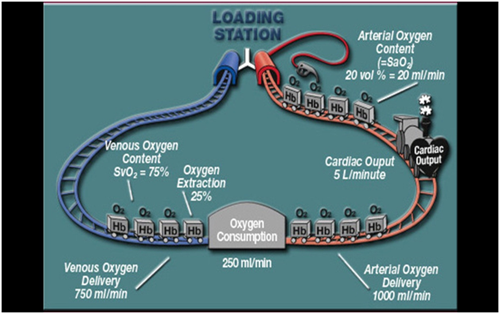
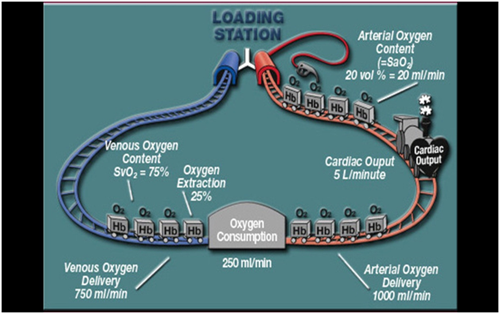
OXYGEN DELIVERY AND EXTRACTION |
| |
Oxygen delivery is determined by the content of the blood and cardiac output: |
| |
 |
PaO2 (PAO2, PaCO2, RQ, atmospheric pressure, K) |
 |
SpO2 |
 |
Hb (affinity of Hb for O2) |
 |
Q |
|
| |
Mechanisms that sustain oxygen flux |
| |
 |
increased oxygen delivery (reflex mechanisms, redirection to essential organs) |
 |
increased extraction ratio |
 |
reduced VO2 (oxygen conservation behaviours) |
 |
anaerobic metabolism |
 |
regional variations |
 |
chronic adaptation |
|
| |
Predicting microvascular flow |
| |
 |
clinical examination |
 |
haemodynamics |
 |
cardiac output based |
 |
clinical ‘tissue perfusion’ indicators |
 |
lactate |
 |
sublingual capillary flow |
 |
SmvO2 |
 |
ScvO2 |
 |
O2 extraction ratio |
 |
central-toe temperature gradient |
 |
gastric tonometry |
|
| |
ScvO2 |
| |
 |
higher extraction suggest stress |
 |
< 40-50% implies tissue dysoxia (high extraction) |
 |
samples upper body venous return largely |
 |
predictive of post op complications and mortality |
 |
suggested target: 65-70% |
|
| |
Processing new results in early goal-directed therapy of sepsis |
| |
The single center, randomized 263-patient Rivers study protocolized EGDT versus usual care in sepsis, back in 2001 had a huge impact around the world. |
| |
This study published more than a decade ago involving patients presenting to the emergency department with severe sepsis and septic shock, mortality was markedly lower among those who were treated according to a 6-hour protocol of early goal-directed therapy (EGDT), in which intravenous fluids, vasopressors, inotropes, and blood transfusions were adjusted to reach central hemodynamic targets, than among those receiving usual care. The ProCESS Investigators conducted a trial to determine whether these findings were generalizable and whether all aspects of the protocol were necessary. |
| |
Ref: A Randomized Trial of Protocol-Based Care for Early Septic Shock. N Engl J Med 2014; 370:1683-1693,May 1, 2014. |
| |
Patient enrollment took place from March 2008 to May 2013, incorporating 31 tertiary US centers. The patient inclusion criteria were essentially identical to the Rivers trial. /td> |
| |
In total, 1,341 patients were enrolled in the trial, split between EGDT (439), protocolized standard therapy (446) and usual care (456). |
| |
The ProCESS Investigators concluded that for patients presenting with early septic shock, in the setting of prompt recognition, prompt intravenous fluid bolus for hypotension, and prompt intravenous antibiotics, there is no apparent additional benefit of protocol-based resuscitation, mandatory central line placement in all patients, or ScvO2 monitoring, with triggers for blood transfusion and dobutamine. |
| |
Source: |
| |
Early Goal Directed Therapy in Septic Shock. |
| |
References and Links |
| |
LITFL |
| |
CCC — Central venous oxygen saturation (ScvO2) |
| |
CCC — Lactate Clearance vs ScvO2 Monitoring in Severe Sepsis |
| |
CCC —SvO2 vs ScvO2 |
| |
Journal articles and textbooks |
| |
1.Dellinger RP, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008 Jan;36(1):296-327. Erratum in: Crit Care Med. 2008 Apr;36(4):1394-6. PubMed PMID: 18158437. [Fulltext] |
| |
2.Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA; Emergency Medicine Shock Research Network (EMShockNet) Investigators. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010 Feb 24;303(8):739-46. PubMed PMID: 20179283; PubMed Central PMCID: PMC2918907. |
| |
3.Jones AE, Brown MD, Trzeciak S, Shapiro NI, Garrett JS, Heffner AC, Kline JA; Emergency Medicine Shock Research Network investigators. The effect of a quantitative resuscitation strategy on mortality in patients with sepsis: a meta-analysis. Crit Care Med. 2008 Oct;36(10):2734-9. Review. PubMed PMID: 18766093;PubMed Central PMCID: PMC2737059. |
| |
4.McKenna M. Controversy swirls around early goal-directed therapy in sepsis: pioneer defends ground- breaking approach to deadly disease. Ann Emerg Med. 2008 Dec;52(6):651-4. PubMed PMID: 19048659. [Fulltext] |
| |
5.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M; Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001 Nov 8;345(19):1368-77. PubMed PMID: 11794169. [Fulltext]. |
FOAM and web resources |
| |
1.ALIEM —Paucis Verbis card: Early goal directed therapy |
| |
2.EMCrit —Severe Sepsis Resources |
| |
3.EMCrit Podcast 14 —EGDT Tirade |
| |
4.EMCrit Podcast 14.5 —A bit more on EGDT |
| |
5.EMCrit Podcast 22 —Non-Invasive Severe Sepsis Care |
| |
6.EP Monthly —Sepsis: EGDT Continues to Deliver versus
Sepsis: Unbundling the Bundle (2012) |
| |
7.EP Monthly — PRO Should Early Goal-Directed Therapy Be the Standard for Sepsis? versus CON Should Early Goal-Directed Therapy Be the Standard for Sepsis? (2010)
|
| |
8.Free Emergency Talks —Emanuel Rivers (USA): Lactate Clearance in Severe Sepsis (2012) |
| |
9.Free Emergency Talks —Emanuel Rivers (USA): Managing Sepsis in the Resuscitation (2012) |
| |
10.Free Emergency Talks — Alan Jones (North Carolina): Optimal Goals of Sepsis (2009) |
| |
11.Free Emergency Talks —Early Goal Directed Therapy – Michael Kuiper (2009) |
| |
12.Free Emergency Talks — Alan Jones vs Nate Shapiro: Is EGDT the standard of care? (2009) |
| |
13.Free Emergency Talks — Peter Greenwald: Early Goal-Directed Therapy in the Community (2010) |
| |
14.ICN — Podcast 33: Delaney on EGDT, Surviving sepsis and ARISE |
| |
15.PulmCCM.org — Surviving Sepsis Guidelines Updated: Preview from SCCM Meeting |
| |
16.PulmCCM.org — Should lactate clearance replace SvO2 in sepsis protocols? (Pro/Con, CHEST) |
| |
17.Surviving Sepsis Campaign |