Conference Lectures
DR SAROJ BANDE, PUNE
Congenital cleft palate repair is a common and painful surgical procedure in infants. As such, children with cleft palate tend to have a compromised airway due to associated congenital anomalies like Pierre Robin syndrome, Treacher Collin syndrome etc. After surgical correction of cleft palate (palatoplasty), children are more prone to develop postoperative respiratory difficulty due to narrowed airway, tongue oedema, increased secretions or bleeding, pain and sedation caused by opioid analgesics(1). Management of their postoperative sedation & analgesia is challenging. On one hand we need to have a quiet baby with no cry or emergence, so that there is less bleeding at surgical site, at the same time we need the baby awake enough to take care of respiration and airway reflexes. Although we have a lot of drugs and techniques to deal with this problem, striking a correct balance can be difficult. Parental presence and reassurance in the recovery room are also known to play a pivotal role.
Recently there is an increasing awareness regarding the need for complete well being of the child in the postoperative period and not just a pain- free state. Sedation and other adverse events produced by opioids do not help in achieving such a goal. In recent times, undisputed supremacy of opioids in treating postoperative pain has been challenged by regional blocks mainly to overcome the side effects of narcotics. Moreover, regional and general anaesthesia techniques are no longer considered as alternative but instead, as complementary. This is especially true in pediatrics where regional anaesthesia is essentially performed under general anaesthesia. The association of the two techniques has dramatically cut down the risks associated with both the techniques. Hodges, Stephens and co-workers while reviewing anaesthesia for cleft surgeries opined that opioids are better avoided and intraoperative and postoperative analgesia can be achieved by local infiltration with local anaesthetics or by nerve blocks(5).
Let us first see the modalities available to us for sedation. Our preoperative assessment will tell us to exclude the babies with chronic airway obstruction or expected airway problems from preoperative sedation. In suitable babies, we may start with a sedative premedication like oral Midazolam 0.5mg/kg if we have trained staff for supervision available with us in the pre & post anaesthesia care unit. This will ensure not only smoother induction & parental separation but will also lead to fair postoperative sedation. Intraoperatively the sedation and analgesia can be provided by IV Fentanyl 1-2 microgm/kg or Morphine 0.05-0.1 mg/kg. Postoperatively we can continue with same drugs as boluses or infusion as required. We must remember that opioids may lead to postoperative drowsiness, respiratory depression and consequent airway compromise & hence cannot be given if there is no trained staff for supervision, pulse oximetry or apnea monitors. Occasionally they may lead to agitation also, increasing the problems further by PONV.
Acetaminophen also can be used individually or in addition to opioids for pain relief. Doses vary as per route of administration. It can be given rectally, 40 mg/kg after induction & then 20 mg/kg 6 hrly. It can be given orally, 20 mg/kg preoperatively & then 10-15 mg/kg 4-6 hrly. Now IV preparations are also available, which can be given 15-20 mg/kg, 6 hrly.
NSAIDs like Diclofenac can be used in infants > 6 months age. Suppository can be used immediately after induction in dose of 1mg/kg. It can be given 1.5 mg/kg, intramuscularly or intravenously in slow infusion. This is observed to be much more effective than Acetaminophen but may increase risk of postoperative bleeding. Hence some advocate their administration 12 hrs after surgery. (2,3)
Now we will see the nerve blocks which can be used for cleft palate repair.
1.Greater palatine Nerve Block -
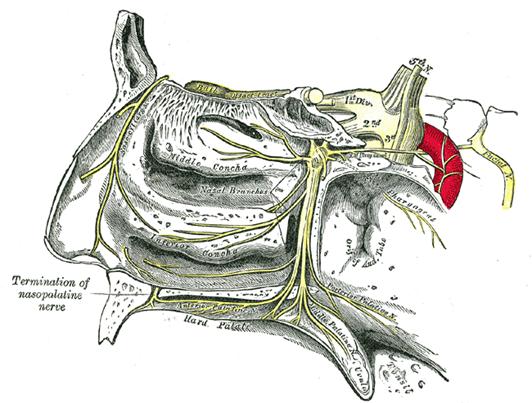
Anatomy :
The greater palatine nerve (anterior palatine nerve) is a branch of the pterygopalatine ganglion that carries both general sensory fibres from the maxillary nerve and parasympathetic fibers from the nerve of the pterygoid canal. It descends through the greater palatine canal, emerges upon the hard palate through the greater palatine foramen and passes forward in a groove in the hard palate, nearly as far as the incisor teeth. It supplies the gums, the mucous membrane and glands of the hard palate, and communicates in front with the terminal filaments of the nasopalatine nerve. While in the pterygopalatine canal, it gives off posterior inferior nasal branches which enter the nasal cavity through openings in the palatine bone, and ramify over the inferior nasal concha and middle and inferior meatuses; at its exit from the canal, a palatine branch is distributed to both surfaces of the soft palate.( Figures 1 and 2) (5)
Figure 1.
 \
\
Figure 2.

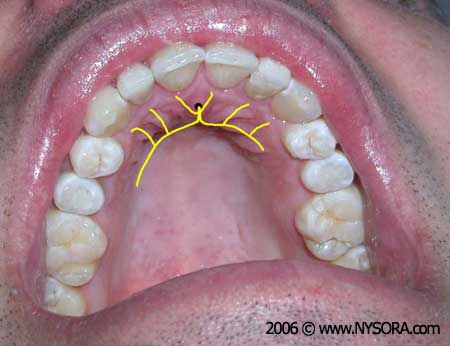
Block procedure : Figure 3(4,5)
Figure 3

The nerve is blocked bilaterally as it exits through the foramen on palatal side opposite the anterior part of the 3rd molar or posterior part of the 2 nd molar tooth. The foramen can be located by pressing a small cotton swab opposite first molar tooth and proceeding posteriorly till it `falls' into a depression created by the foramen. A thin, short-bevelled needle is inserted from opposite side of the mouth at right angles into this depression and about 0.6 to 1 ml of 0.25% bupivacaine or 0.2 % ropivacaine is injected after negative aspiration for blood. Alternatively, to minimize failures, an open technique may be tried. That is, infiltrating the nerve under direct vision after the elevation of palatal flap, which is part of surgery. Though majority of palatal mucosa is innervated by greater palatine nerve it also derives supply from lesser palatine and nasopalatine nerve. All are branches of maxillary nerve. During surgery, nasopalatine nerve is divided as it exits through the foramen. The lesser palatine nerve which supplies the soft palate lies in close proximity to greater palatine nerve in the canal before the latter comes out of the foramen. As we inject local anaesthetic into the foramen we might block the maxillary nerve itself or its branches which may explain the total analgesia of the palate. Greater palatine nerve block is easy to learn and to perform with very high success rate. It is very effective in producing postoperative analgesia without any significant adverse events. Moreover it produces prolonged analgesia even upto 24 hrs with addition of additives like Dexmedetomidine (6). By employing regional techniques we not only make the patient's stay in the postoperative period comfortable, but also avoid many serious adverse events associated with traditional analgesic regimens. It also facilitates early feeding.
2.Bilateral suprazygomatic maxillary nerve block
This new approach of maxillary nerve Block presents several advantages compared to other blocks. The infrazygomatic approach incurs a risk of vascular puncture due to vicinity of inframaxillary artery whereas suprazygomatic approach from frontozygomatic angle is safer because the maxillary artery in pterygopalatine fossa lies ventrally & inferiorly to the maxillary Nerve. Also, there is no risk of penetrating skull base or orbit, unlike infrazygomatic approach. Safety of block can be further increased by using nerve stimulator- seeing contraction of temporalis muscle. Local anesthetic injected can be 0.15 ml/kg of 0.2% ropivacaine . Bilateral SMB is an easy regional anesthesia technique that reduces total morphine consumption at 48 h after cleft palate repair in children and the use of continuous infusion of morphine and may decrease postoperative respiratory complications. (7,8)
3.Nasopalatine nerve block (5)
Figure 4.
 .
.
In short, the tricky problem of postoperative sedation & analgesia can be solved successfully by using a multimodal approach after proper assessment of the patient.
References:
- Dr Ellen Rawlinson, POSTOPERATIVE AIRWAY COMPLICATIONS AFTER CLEFT PALATE REPAIR, ANAESTHESIA TUTORIAL OF THE WEEK 237, 22ND AUGUST 20.
|
||
- Manjunath R Kamath, Sripada G Mehandale, US Raveendra, Comparative Study of Greater Palatine Nerve Block and Intravenous Pethidine for Postoperative Analgesia in Children Undergoing Palatoplasty, Indian Journal of Anesthesiology CLINICAL INVESTIGATIONS, 2009, Vol 53, issue 6, Page 654-661,
- www.NYSORA.com
|
||
Mesnil M, Dadure C, Captier G, Raux O, Rochette A, Canaud N, Sauter M, Capdevila X, A new approach for peri-operative analgesia of cleft palate repair in infants: the bilateral suprazygomatic maxillary nerve block., Paediatr Anaesth. 2010 Apr;20(4):343-9.
- Chiono, Julien M.D.; Raux, Olivier M.D.; Bringuier, Sophie Pharm.D., Ph.D.; Sola, Chrystelle M.D.; Bigorre, Michèle M.D.; Capdevila, Xavier M.D., Ph.D.; Dadure, Christophe M.D., Ph.D. Bilateral Suprazygomatic Maxillary Nerve Block for Cleft Palate Repair in Children: A Prospective, Randomized, Double-blind Study versus Placebo, Anesthesiology: June 2014 - Volume 120 - Issue 6 - p 1362–1369.