Conference Lectures
- Introduction
Modern anesthesiology manages reflexes associated with surgery and disrupts the pathway of noxious stimulus to the brain. Avoiding the painful stimulus in the first place can do this, but this is unrealistic in a surgical setting. Next best, then, is “hiding” the surgical stimulus from the ever-vigilant spinal cord. We can block the nociception receptors from transmitting a message of pain to the brain by injecting local anesthetic agents into the surgical field, or by blocking the nerves that relay the message of pain to the spinal cord and brain. That is the prime use of regional anesthesia in modern practice. Common shoulder procedures include Hemiarthroplasty, Total shoulder arthroplasty, Shoulder arthroscopy, Subacromial decompression, Shoulder instability procedures such as rotator cuff repair
- Shoulder anatomy and innervations
The shoulder girdle consists of three joints and one articulation: sternoclavicular joint, acromioclavicular joint, glenohumeral joint (shoulder joint), and scapulothoracic articulation. The muscles and ligaments of the shoulder allow and restrict movement along with providing active and passive stabilization of the shoulder. Biomechanically, the shoulder has three degrees of freedom and the muscles act at the shoulder to permit particularly free motion: flexion, extension, abduction, circumduction, internal rotation, and external rotation. Static stability of shoulder is provided by the labrum, capsule, and glenohumeral ligament while dynamic stability is provided by the rotator cuff, long head of the biceps tendon, and periscapular muscles.
Figure 1. Brachial plexuses


Table 1: Distribution of the Brachial Plexus
The shoulder area is innervated by nerves of both cervical and brachial plexuses. The former supplies the skin above the clavicle, shoulder tip, and first two intercostal spaces anteriorly through the superficial cervical plexus and supraclavicular nerves (C3-C4).
The suprascapular nerve: The suprascapular nerve supplies sensory innervations to the subacromial bursa, acromioclavicular joint, coracoclavicular ligament, and 70% of the shoulder joint capsule. This nerve arises from the superior trunk of the brachial plexus, C5-C6 and possibly C4. The suprascapular nerve descends posteriorly, passing through the scapular notch, innervating the supraspinatus and infraspinatus muscles. It provides sensation for the posterior shoulder capsule, acromioclavicular joint, subacromial bursa, and coracoclavicular ligament.
The axillary nerve: The axillary nerve originates from C5-C6 nerve roots, with occasional contribution from C4. It is derived from the posterior cord of the brachial plexus. The axillary nerve crosses the anteroinferior aspect of the subscapularis muscle where it crosses posteriorly through the quadrilateral space and divides into two trunks. The anterior trunk supplies the motor innervations to the anterior and middle deltoid muscle. The posterior trunk gives off a branch to the teres minor muscle and the posterior deltoid muscle before terminating as the superior lateral brachial cutaneous nerve, which supplies the cutaneous inervation to the skin overlying the deltoid muscle.
- Regional anesthesia techniques for shoulder surgery
- Interscalene Block
- Suprascapular nerve Block
- Supraclavicular Block
- Subacromial block / intra-articular injection
- Interscalene Block
The interscalene block is the most commonly used block for shoulder procedures. This approach blocks the brachial plexus at the nerve root or trunk level. The block is especially useful for procedures involving the shoulder, including the lateral two-thirds of the clavicle, proximal humerus, and shoulder joint. The interscalene block is performed as a single-injection or continuous peripheral nerve block. The block is done using the paresthesia technique, nerve stimulation technique, ultrasound guidance, or nerve stimulation-ultrasound combination.
Figure 2. Anatomical landmarks of interscalene block
Classical Approaches
The classic approach of Winnie, which is considered the anterior approach, is still commonly performed. The technique is performed by palpating the interscalene groove at the level of the cricoid cartilage (C6 vertebra). The needle is directed medially, slightly caudal, and slightly posterior (toward the contralateral elbow) while seeking to elicit a paresthesia in the C5-C6 nerve distribution as the endpoint for injection.
Other Techniques:
Meier used the same landmarks, but enters the skin at 30 degrees and 2-3cm cephalad to the Winnie approach. The needle is directed toward the middle to lateral third of the clavicle to reduce complications and facilitate placement of catheters.
Borgeat and Ekatodramis also modified the Winnie approach. In this case, the needle is inserted approximately 0.5cm below the level of the cricoid and directed 45–60 degrees toward the interscalene groove.
Chan used ultrasound to directly visualize the nerve roots of the brachial plexus in the interscalene groove at the level of cricoids.
Posterior Approaches
The posterior approach to the interscalene blockade -passing the needle between the levator scapulae and the trapezius muscle to reduce neck pain, which was thought to be due to the needle entering the extensor musculature..
Advantage:
When using the cervical paravertebral approach, the catheter is better anchored because it passes through multiple layers of muscle and vital anterior structures have less risk of being injured.
Disadvantage:
The major disadvantage of the cervical paravertebral approach is the distance the needle must travel to reach target. The needle must pass through multiple muscle layers which may be painful to the patient. Also, the needle passes through the middle scalene muscle where injury to the long thoracic and dorsal scapular nerves could occur.
Complications
Common complications of the interscalene nerve block include phrenic nerve blockade (hemidiaphragmatic paresis), Horner’s syndrome, recurrent laryngeal nerve blockade, and vasculature puncture (hematoma). Rarer, but potentially devastating, complications include carotid artery puncture and intervertebral artery injection, pneumothorax, subdural injection, intervertebral foramina injection resulting in spinal or epidural anesthesia, and nerve injury. In addition, indwelling catheters may become infected, kinked, knotted, or entrapped. The risk for most of these complications is minimized by awareness of the location of the needle and surrounding structures. This is facilitated with ultrasound guidance.
Voermans et al. reported a case of permanent loss of cervical spinal cord function associated with the posterior approach to the interscalene block. This was thought to be due to a direct intrathecal and intramedullary injection.
Benumof reported four cases in which the performance of interscalene block during general anesthesia was followed by total spinal anesthesia and extensive permanent loss of bilateral cervical spinal cord function.
- Suprascapular Nerve Block
The suprascapular nerve block combined with an axillary nerve block may provide an efficacious alternative to the interscalene nerve block for shoulder anesthesia. The axillary nerve block as described in this section refers to blockade of a terminal branch of the brachial plexus, the axillary nerve. As previously mentioned, the majority of the nerve supply to the shoulder is provided by the suprascapular and axillary nerves. When these nerves are blocked separately, there may be fewer complications and side effects than the traditional interscalene block. The phrenic nerve is not blocked; therefore, these blocks may be used for patients that are not candidates for an interscalene block, for example, severe chronic obstructive pulmonary disease or contra-lateral hemidiaphragmatic paresis. This technique may also be used as a rescue block for unsuccessful interscalene blocks. A disadvantage of these blocks is that branches proximal to the injection site or regions not innervated by these nerves are not blocked. This may leave analgesia to the surgical region incomplete, requiring supplementation by intravenous analgesics, local anesthetic infiltration, or general anesthesia.
Figure 3. Anatomical landmarks of Suprascapular Block

Approaches
For the suprascapular nerve block, the ideal approach ensures blockade of the more proximal branches to the acromion and the subacromial region to maximize coverage. This may be achieved by blocking the nerve in the suprascapular notch; however, this location is associated with a small risk of pneumothorax. Price described a technique for this block that was adopted from Meier et al. in which the suprascapular nerve is blocked as it travels across the supraspinous fossa. Price described a technique to block the axillary nerve immediately after it passes through the quadrilateral space as it lies just posterior to the humerus.
Checcucci et al. also described techniques for blocking the suprascapular and axillary nerves. The suprascapular nerve is blocked by eliciting a supraspinatus and infraspinatus motor response (arm abduction and external rotation) after inserting a nerve-stimulating needle at a point 2cm medial to the medial border of the acromion and approximately 2cm cephalad to the superior margin of the scapular spine. The axillary nerve is blocked by drawing a line between the lateral-posterior angle of the acromion and the olecranon tip of the elbow. A perpendicular line is drawn from this line to the axillary fold. A nerve-stimulating needle is inserted 2cm cephalad to the intersection of the lines and a deltoid muscle motor response is sought to identify the axillary nerve. Matsumoto et al. developed a technique for performing the suprascapular nerve block based upon cadaveric anatomy. The insertion point is the midpoint of the anterolateral angle of the acromion and the medial edge of the scapular spine. The needle is inclined at a 30-degree angle dorsal to the coronal plane (axis of the body) and inserted until it reaches the base of the coracoid process. The ultrasound probe, oriented transversely to the scapula spine, is moved cephalad and lateral to directly visualized and inject around the nerve in the suprascapular notch.
Complications
The suprascapular or the axillary nerve blocks have the basic risks of any peripheral nerve block: nerve injury, intravascular injection, and vascular puncture. In addition, the suprascapular block may have a small risk of a pneumothorax.
- Supraclavicular Block
Supraclavicular block provides anesthesia of the entire upper extremity in the most consistent, time-efficient manner of any brachial plexus technique. The “divisions” of the brachial plexus are blocked. Similar to the interscalene nerve block, the block is done between the anterior and middle scalene muscles. The popularity of this approach was limited in the past due to the risk of pneumothorax when using landmark-based techniques. However, ultrasound has rejuvenated interest in this block by providing real-time visualization of the target tissues and surrounding structures, potential reducing complications such as pneumothorax and nerve injury. The block is frequently used for elbow, forearm, wrist, and hand surgery. Since it is performed above the clavicle, it can also provide shoulder analgesia. The concern with using this block for shoulder surgery is that proximal nerves and nerve branches that supply the shoulder may be missed.
Figure 4. Anatomical landmarks of Supraclavicular block
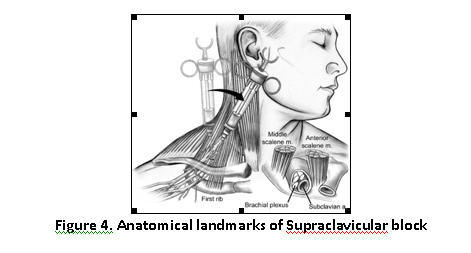
Approaches
The supraclavicular block can be performed by two landmark-based techniques, classic approach and plumb-bob approach. Using the classic approach, the needle entry point is 1cm superior to the clavicle, at the midpoint of the clavicle. It is advanced approximately parallel to the patient’s neck and head, from cephalad to caudad toward the first rib. The plumb-bob technique uses an anterior-to-posterior trajectory of the needle to reduce the risk for pneumothorax. With either method, the paresthesia technique or nerve stimulation technique may be used to determine the endpoint for injection
Complications
Complications of supraclavicular block include pneumothorax (0.6%–6.1%), vascular puncture, intravascular injection, Horner’s syndrome, recurrent laryngeal nerve blockade, nerve injury, and phrenic nerve blockade with transient hemidiaphragmatic paresis.
- Subacromial Block/Intra-Articular Injections
The subacromial block is generally used for arthroscopic shoulder procedures including subacromial decompression and rotator cuff repair. The pain for these procedures can vary from mild to severe. Therefore, single-injection or continuous infusions are employed depending on the anticipated intensity of the pain. Single-injection and continuous infusions of local anesthetic in the subacromial space have been shown to provide superior pain relief compared to placebo. The advantages of subacromial injection (infusion) compared to an interscalene block (infusion) include easy and rapid catheter placement, direct visualization to facilitate proper placement, and little to no extremity numbness or weakness.
Intra-articular injections have many of the same advantages as a subacromial block. However, the efficacy of these injections for postoperative pain management has recently been questioned.
Figure 5. Anatomical landmarks of subacromial block
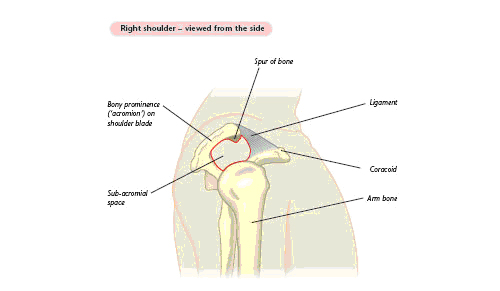
Approaches
A subacromial continuous infusion catheter is placed intraoperatively by the surgeon. At the end of the arthroscopy, the posterior portal is used to visualize the subacromial space. Under direct visualization, the catheter sheath is inserted posterolaterally, and several centimeters of catheter are placed in the subacromial space. An elastomeric pump is connected to the catheter for outpatient use. The patient discontinues the pump at home by removing the dressing and catheter. Single injections are done in the same manner without placing the catheter. In the case of intra-articular injections, the glenohumeral joint is directly injected with a local anesthetic, opioid, or combination. This is easily done with direct visualization during arthroscopy.
Complications
One of the advantages of the subacromial injection or infusion may be a lower complication rate in comparison to the interscalene nerve block. Also, there is less risk of extremity numbness or weakness. subacromial pain pumps used for arthroscopic shoulder procedures are safe in the short term. Recently, there has been concern about chondrolysis or rapid articular cartilage destruction related to intra-articular injections. Local anesthetics have been shown to induce chondrotoxicity in animal studies, especially when bupivacaine is used in high doses. This is a devastating complication in a young patient and difficult to manage
Table 2: Common Problems during Nerve Localization and the Corrective Action

Conclusion
The interscalene brachial plexus block remains the mainstay for shoulder surgery. It is especially beneficial for shoulder surgery causing moderate-to-severe pain. For cases in which pain is anticipated to last for several days, a continuous interscalene block is appropriate. In all the outcome studies in this paper, the interscalene block produced superior analgesia to other techniques. For mild pain, other methods may be considered, but it is still unclear how much benefit these techniques offer in comparison to oral analgesics. When an interscalene block is contraindicated, the suprascapular and axillary nerve blocks offer a reasonable alternative. Since these techniques have not gained widespread use, providers may be less familiar with how to perform them. The suprascapular and axillary nerve blocks appear safe and should be added to the anesthesia provider’s skill set. The use of ultrasound in the last five years has enhanced regional anesthesia. Ultrasound-guided upper extremity blockade often provides faster block performance, faster block onset, and greater block success compared to the nerve stimulation technique, while providing a similar safety profile. Finally, intra-articular injection of local anesthetic is not recommended because of the association with chondrolysis.
Bibliography
- Christina L.Beecroft, FRCA, FDS RCS, David M. Coventry, FRCA, “Anesthesia for shoulder surgery”, Oxford Journals, Volume 8, Issue 6 Pp 193-198
- Clifford Bowens Jr. and Ramprasad Sripada, “Regional Blockade of the Shoulder: Approaches and Outcomes”, Review article, Hindawi Publishing Corporation, Volume 2012, Article ID 971963
- Andre P. Boezaart and Patrick Tighe, “New trends in regional anesthesia for shoulder surgery: Avoiding devastating complications”, Int J Shoulder Surg. 2010 Jan-Mar, 4(1): 1-7
- http://www.nysora.com
- Campbell operative orthopedics
- Turek text book of orthopedics
- Rockwood and Green text book of trauma and orthopedics