Conference Lectures
DR SURAJIT GIRI
Consultant Anaesthesiologist
Executive committee member
Academy of Regional Anaesthesia (AORA)
Sivasagar
Assam
INTRODUCTION:
It is now a known fact that day-by-day road traffic accidents are increasing. Patients present to us with multiple levels of injuries from long bones, vertebrae to rib fracture! They are in severe pain and agony for multiple injuries! As Anaesthesiologist we know that simple analgesics starting from intravenous to oral is not sufficient to control these acute pain.
Today RA is well-established technique for analgesia and anaesthesia in trauma (2, 3, 4). Neuraxial and peripheral nerve blocks are most effective methods for acute pain treatment. Peripheral nerve stimulation (PNS) and recent advances in ultrasound-guided nerve blocks make those procedures safer. RA has numerous advantages than systemic analgesics in acute trauma. A well-conducted RA is much safer than other modalities of analgesia with minimal to zero systemic effects! Several studies showed that RA hasten recovery, decrease intensive care unit and hospital length of stay, improve cardiac and pulmonary function, decrease infection rates, decrease sympathetic activation and promotes earlier return of bowel function (5, 6). Lack of systemic effects, no effects on mental status and no to minimal changes of hemodynamics makes RA attractive choices in trauma patients (2, 4, 5). Simple peripheral nerve blocks can be done in prehosiptal setting or in the emergency department, which decreases the pain and stress due to trauma, which improves patient’s comfort and decreases the probability of chronic pain development (2, 4, 5, 7, 8).
This write up will not discuss about details of techniques of various RA. I shall try to cover up some key issues in acute trauma only. For detailed discussion on techniques, LA drugs and volumes, readers are advised to follow any standard textbook. Myself from a small district of Assam, I don’t have access to USG! Most of the blocks described here are performed by PNS including catheter insertion except TAP, FICB and RSB (Rectus sheath block), which are done absolutely by LOR!
WHY THERE IS NEED TO CONTROL THE ACUTE PAIN?
- To prevent the progression from acute to chronic post –trauma pain!
- To prevent the metabolic responses following acute traumatic pain!
- To blunt the autonomic responses – as you know following trauma, the sympathetic nervous system is activated, causing an increase in plasma levels of epinephrine and norepinephrine, which leads to CVS responses including tachyarrhythmia!
TEN MUST PREREQUISITE FOR RA IN ACUTE TRAUMA
1.ABC: Airway, Breathing and Circulation are first to be addressed including cervical injury.
2.Assessment of organ injuries including blunt abdominal trauma.
3.Mental status. Glasgow Coma Scale (GCS)
4. 1, 2, 3 addressed, then plan for RA. Associated neurovascular injury to be documented.
5. All resuscitative equipments are available.
6.At least 5-10 bottles of Lipids in the cart for Local anaesthetic systemic toxicity (LAST).
7.Recapitulation of Regional anaesthesia anatomy of the injured area including cutaneous distributions and sparing effects of a particular nerve block.
8.Choose an Ideal RA technique considering all injured limbs!
9.Duration of the surgical procedure and comfort ability of the patient!
10. Written informed consent including possible complications from attendants.
WHICH IS BETTER? BLIND, PNS OR USG?
BLIND TECHNIQUE
It requires excellent knowledge of the anatomy and experience of the Anaesthesiologist. The failure rates are high compared to PNS or ultrasound-guided techniques. Advantages are no painful muscle contractions are elicited and the technique requires no expensive equipment. May be very useful in remote areas or during military wars or disasters.
PERIPHERAL NERVE STIMULATOR TECHNIQUE (PNS)
The disadvantage is that a motor response is required to confirm needle position, which may be undesirable in an acute trauma patient. For example, nerve damage distal to the injection site can prevent the anticipated muscle contraction even with the needle is in close proximity to the nerve. The resulting muscle contraction can be extremely painful and sometimes potentially causes further damage.
ULTRASONOGRAPHY
Today it is the gold standard! Disadvantages are the availability and cost factor for district level hospital and it needs further expertise for nerve blocks! But if someone have access to it, scanned the nerve and put the LA around it! In this technique we can effectively provide anaesthesia and analgesia even with a very small volume of LA.
RA FOR UPPER LIMB TRAUMA:
Depending upon the site of fracture and injury and associated comorbid condition of the patient we can choose interscalene, supraclavicular, infraclavicular, axillary to selective nerve block at the level of elbow. Nerve block approaches depend upon the site of injury and distribution of anaesthesia by a particular nerve block technique.
KEY ISSUES
The supraclavicular nerves are branches of the superficial cervical plexus (C3–C4) (Fig A) and provide cutaneous innervation of the cape of the shoulder. It is not a part of the brachial plexus. They are consistently blocked by interscalene (IS) approach. However, they may require separate blockade if shoulder surgery is planed using more distal approaches of brachial plexus.
In spite of IS block for surgery on the clavicle, one have to block supraclavicular nerve (Fig A) for complete analgesia and anaesthesia. A line is drawn between mastoid process and clavicular insertion of sternocleidomastoid muscle (Fig). Midpoint of this line is taken just posterior to sternocleidomastoid muscle where supraclavicular branches arises (Fig B, C). To block this nerve few ml of subcutaneous LA infiltration is enough (Fig), which completes the anaesthesia and analgesia for clavicular surgery.
Intercostobrachial nerve is not part of the brachial plexus. It is a branch of the second intercostal nerve; it is not anesthetized by plexus block. It supplies the inner medial upper part of arm (Fig) The intercostobrachial nerve (T2) requires separate blockade for surgeries of the medial upper arm or axilla. It has to be blocked separately if incision lies over that area. Subcutaneous few ml of LA infiltration over the upper medial arm is sufficient.
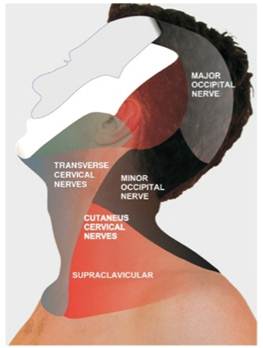
Fig : A : SUPRACLAVICULAR NERVE AND INNERVATION AREA
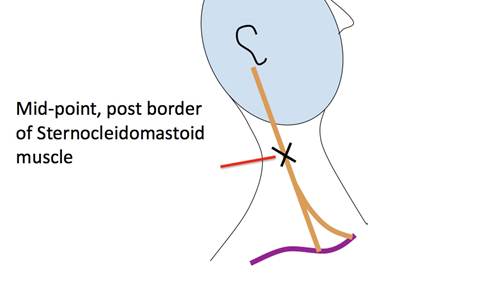
Fig B: Injection point for supraclavicular nerve.
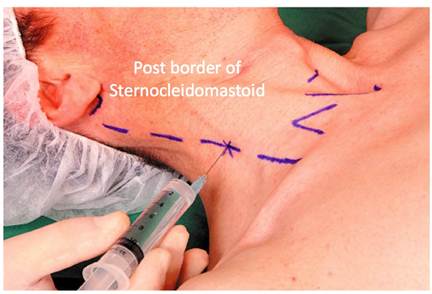
Fig C: Supraclavicular nerve injection technique.

Fig D: T2 Intercostobrachial nerve supply area.
Key Issues
In Clavicular fracture there is risk of supraclavicular nerve injury, it also applies to radial nerve injury in shoulder dislocation and supracondylar fracture of humerus. Before block placement always check for these nerves for possible preexisting nerve injuries! Document the detailed nerve injury in the case sheet, discuss and declare with the family members and then only proceed for RA with an informed written consent!
RA FOR LOWER LIMB TRAUMA
Several studies described better pain control, reduce incidence of DVT, decrease incidence of postoperative pneumonia in patients with femur and hip fractures managed with RA (10, 11). Approaches can be chosen according to the regional anaesthesia anatomy of the traumatic limb. Both Fascia Iliaca Compartment (FICB) and femoral nerve block is an attractive choice with catheter in situ. Femoral nerve can be blocked at lumbar area by posterior lumbar plexus technique, at inguinal ligament level by FICB and at inguinal natural cease level by simple femoral nerve bock. Table 1 compares the all approaches.
Sciatic nerve block is indicated for more distal femur fracture and fractures of le, ankle, heel and sole surgery. There are multiple approaches to sciatic nerve from proximal in buttock to distal at popliteal level. Beauty of sciatic nerve block is that we can block this nerve in various positions from supine, lateral, prone, lithotomy position. According to patient comfort we can place the block.
For finger and sole debridement and surgery one can think of ankle block also. Disadvantages of ankle block are it requires multiple injections for complete anaesthesia and analgesia, which may not be acceptable to already traumatized patient.
KEY ISSUES
According to regional anaesthesia anatomy we have to choose intelligently the approach and necessary nerve blocks. Like, lower end of femur is supplied by femoral, obturator and sciatic nerve (Fig3)! For lower end of femur plating incision comes at the lateral side of lower thigh and this area is supplied by lateral femoral cutaneous nerve. Therefore the ideal PNB would be Lumbar Plexus Block (LPB) plus sciatic nerve block.
IDEAL NERVE BLOCK TECHNIQE FOR COMMON LOWER LIMB SURGERY
A.Hemi replacement arthoplasty (HRA) for fracture neck femur = LPB plus classical sciatic plus upper part of incisional area above greater trochanter (GT) infiltration by few ml of LA whether by surgeon or anaesthetist as this part are supplied by lateral cutaneous branch of the iliohypogastric nerve. Simple LA infiltration is sufficient.
B. Dynamic Hip Screw for trochanteric fracture femur (DHS)= Femoral plus lateral femoral cutaneous nerve plus sciatic nerve or LPB plus sciatic. Disadvantage with only PNB for DHS is that patient have to lie flat on the ortho table and patient feels discomfort in the no blocked normal limb to outstretch the normal limb. Therefore patient needs comfort whether by sedation like propofol or demedetomidinre infusion.
C.Lower end of femur=LPB plus sciatic is ideal.
D.Tension Band Wiring (TBW) of patella= Femoral nerve block
Patellectomy= Femoral plus sciatic.
E. Below knee surgery= Sciatic plus femoral or saphenous nerve.
Fascia iliaca vs. femoral vs. lumbar plexus block –
|
Fascia Iliaca |
Femoral |
Lumbar Plexus |
Instruments |
No: needle / epidural needle and syringe |
Yes PNS or USG |
Yes PNS/USG |
Expertise |
No to Minimal |
Yes+ |
Yes +++ |
Volume of LA |
35-40ml |
20ml |
15-20ml |
Intensity of nerve blocking capacity |
Femoral +++ |
Femoral +++ |
Femoral+++ |
Positioning |
No need: Supine |
No need: Supine |
Lateral position |
Comfort to the pat |
+++ |
++ |
__ |
Success rates |
++ |
+++ |
++++ |
Complications |
Very few |
+ |
+++ |
Table 1 = Comparison of Fascia Iliaca, Femoral and lumbar plexus block
TIBIAL FRACTURE
Tibial fractures are usually associated with high-speed trauma like motor vehicle accident. Open fractures are treated operatively but closed fractures are managed by closed reductions depending upon the fracture pattern and instability! In such fracture we have to look for Acute Compartment Syndrome (ACS).
KEY ISSUES
Acute Compartment Syndrome
Acute compartment syndrome (ACS) is a very dangerous complication in extremity injury, characterized by acute and rapidly progressive neurological and muscular dysfunction associated with an increase in intra-compartmental pressure in an injured extremity. ACS can occur in any closed fascial compartment in the upper or lower extremity. Incidence following Tibial fracture is approximately 7% (ranging from 2.7% to 11%) while forearm and elbow injuries account for 8.5% of ACS. Results are satisfactory if diagnosis is done early and treated aggressively. It has potentially devastating sequeale; therefore the regional anesthesia should be used very carefully for fixation of extremity surgery.
Pathophysiology of ACS
An initial insult causes tissue ischemia in the affected fascial compartment. The insult causes increase in pressure, which leads to transient ischemic injury leading to an inflammatory process whereby local edema ensues, which causes an increase in swelling. Eventually, the intra-compartmental pressure becomes sufficiently high and it prevents blood flow through the low-pressure capillary system in the affected tissues. Tissue perfusion is decreased further, which worsens the local ischemia. It leads to a vicious cycles of increased pressure èischemia èmore release of mediators èincrease in vascular permeabilityè increase in edema èincreased pressure.
Normal tissue pressure is 0-10mmHg.
HOW TO DIAGNOSE ACS?
By clinical signs and symptoms, but sometimes it is unreliable. One has to look for different signs and symptoms! But in uncooperative or sedated and ventilated patient it is very difficult to diagnose ACS! One should have high index of suspicion in selected high-risk patients!
|
Pain |
Paraesthesia |
Pain with passive stretch |
Paraesthesia |
Most Reliable sign |
3 |
5 |
5 |
2 |
Subjective unreliable sign |
4 |
3 |
3 |
3 |
Earliest sign |
8 |
4 |
2 |
0 |
Latest Sign |
0 |
5 |
0 |
5 |
Table: 2: Ulmer T. Journal of Orthopedic Trauma 2002; 16(8): 572-7)
Non-clinical monitors for compartment syndrome
- Compartment pressure monitoring
Easy, but continuous values are more important than single value. Needs a special device.
- Near infrared spectroscopy.
Noninvasive but expensive; useful only for shallow surfaces! Does not measure the deep posterior compartment of calf.
- Creatine phosphokinase
Again Cheap, readily available but late indicator, damage already been done. Confusing also in polytrauma patients, as other muscles injury also increases the level.
TREATMENT FOR ACS?
Immediate Fasciotomy and release the tissue pressure! It is an urgent surgery!
RA IN BLUNT CHEST TRAUMA
We are regularly getting patients of pulmonary contusion and multiple rib fractures! Mortality increases if there is increase numbers of ribs fractures rising 10% for three ribs to >30% for six or more ribs. Likewise morbidity increases dramatically if there are concomitant pulmonary contusions. Rib fractures are very painful limiting ability to breath leading to inadequate cough, atelectasis, pneumonia and respiratory failure.
RA TECHNIQUE |
ADVANTAGES |
DISADVANTAGES |
Thoracic epidural |
Easy |
Hypotension |
Paravertebral block |
Excellent UL analgesia. |
Small risk of pneumothorax |
Intercostal nerve block |
Very easy |
Requires multiple injections |
Intrapleural block |
Easy if there is in situ chest tube |
Effectiveness variable |
Table3: Various techniques of RA for rib fracture.
REGIONAL ANALGESIA IN ABDOMINAL TRAUMA
TECHNIQUE |
ADVANTAGES |
DISADVANTAGES |
Thoracic epidural |
Excellent choice |
Coagulation disorder |
Paravertebral |
Excellent |
Multiple injections |
Transversus abdominis plane block (TAP) |
Easy |
Covers upto parietal peritoneum |
Rectus sheath block |
Easy |
If incision crosses midline BL block! |
CONCLUSION
RA in trauma has its own great impact with numerous advantages. RA increases patient safety, controls the acute traumatic pain quite effectively and decreases the chances to progression to chronic posttraumatic pain. With the advent of nerve stimulator and now with USG it is becoming easier and much safer to do a nerve block. Different RA techniques can be used in different phase of the trauma. Like FICB in the field, intercostal nerve block in emergency department to epidural catheter for operating room and paravertebral catheter in ICU in same patient.
It is important to assess the associated injuries, hemodynamic stability and mental status before proceeding for any RA technique and as Anaesthesiologist it is our duty to choose accordingly the best possible RA technique including multiple nerve block catheter in same patient for relief of pain and agony.
Hope in coming year USG will be in every hand of Anaesthesiologist, by which we can simultaneously assess or scan for associated injuries and place nerve block catheter in multiple places in acutely multi level traumatized patient. Though USG is gold standard in today’s world of anaesthesia, still LOR and PNS blocks are equally effective in limited resource area, if practiced regularly and one have enough of knowledge and understanding of regional anaesthesia anatomy and have access to equipment and drugs to treat any after block complications irrespective of different techniques for RA.
REFRERENCES
1.Regional anaesthesia in trauma – A case based approach - Jeff Gadsden
2.DAVIDSON E M, GINOSAR Y, AVIDAN A 2006 Pain mana- gement and regional anaesthesia in the trauma patient. Curr Opin Anaesthesiol 18: 169–174
3.LUCAS S D, LE WENDLING L, ENNEKING F K 2012 Regional Anesthesia for the Trauma Patient. In: Racz G (ed.) Pain Management - Current Issues and Opinions. InTech, Rijeka, p 261-277
4.WU J J, LOLLO L, GRABINSKY A 2011 Regional Anesthesia in Trauma Medicine. Anesthesiol research pract: 1-7
5.MALCHOW R J, BLACK I H 2008 The evolution of pain mana- gement in the critically ill trauma patient: emerging concepts from the global war on terrorism. Crit Care Med 36 (supp 7): S346–S357
6.LUGER T J, KAMMER LANDER C, GOSCH M, LUGER M F, KAMMERLANDER-KNAUER UROTH T 2010 Neuroaxial versus general anaesthesia in geriatric patients for hip fracture surgery: does it matter? Osteoporos int 21: S555-572
7.BULGER E M, EDWARDS E M, KLOTZ T, JURKOVICH G J 2004 Epidural analgesia improves outcome after multiple rib fractu- res. Surg 136: 426-430
8.MOON M R, LUCHETTE F A, GIBSON S W, CREWS J, SU- DARSHAN G, HURST J M 1999. Prospective, randomized com- parison of epidural versus parenteral opioid analgesia in thoracic trauma. Ann of Surg 229: 684-691
9.ASRA NEWS 2013. ACS –CAUTION AHEAD
10.BEAUDOIN F L, NAGDEV A, MERCHANT R C, BECKER B M 2010 Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures. Am J Emerg Med 28: 76–81
11.MON ZON D G, ISERSON K V, VAZQUEZ J A 2007 Single fascia iliaca compartment block for post-hip fracture pain relief. J Emerg Med 32: 257-262
12.Regional anaesthesia for trauma patients: DINKO TONKOVI , NJA NESEK ADAM, ROBERT BARONICAD, ANIJELA BANDI ,PAVLOVI ELJKO DRVAR TAJANA ZAH BOGOVI.
13. DR SHIV KUMAR SINGH Liverpool , UK – Images of lower limb innervation and FICB.
14.Admir Hadzick - Textbook of Regional Anesthesia and Acute Pain Management 2007
15.David L Brown Atlas of Regional Anaesthesia , 3rd Edition.
16.www.nysora.com