Conference Lectures
INTRAOPERATIVE FLUIDS: HOW MUCH IS TOO MUCH?
PROF.B.KALA.MD, DA,DIRECTOR & HOD, INSTITUTE OF ANAESTHESIOLOGY AND CRITICAL CARE, MADRAS MEDICAL COLLEGE, CHENNAI-03, INDIA.
Introduction:-
Fluid management has been used for more than two hundred years and is essential part of patient care in the perioperative period. Adequate plasma volume is vital in maintaining cardiac output and hence tissue perfusion. Inadequate tissue perfusion is associated with poor outcome following surgery. All surgical patients must have intravenous access which is considered as life line and require peri operative intravenous fluid therapy.
Administration of intravenous fluid is equivalent to one kind of drug therapy and potentially harmful if not prescribed appropriately. Inadvertent intra operative over hydration is the cause for post operative problems such as delayed recovery, delayed wound healing, tissue edema, lung water accumulation which may end in morbidity and mortality .
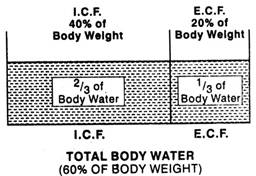
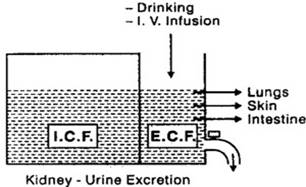
DISTRIBUTION OF BODY FLUIDS :-- (fig-1) HOW BODY MAINTAINS WATER BALANCE? ( Fig-2)
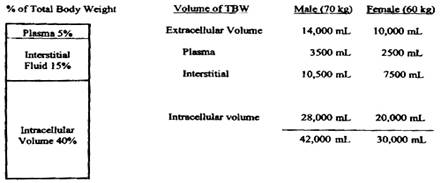
DIFFERENT FLUID COMPARTMENTS:-- ( FIG -3)
A 70 kg adult male having blood water of 42 litres(60% of body weight), Of this (2/3) 28L intra cellular, & (1/3)extra cellular volume is 14L ECV. This is further divided into plasma -3.5L and interstitial -10.5L.
Why we should administer peri operative IV fluids?
- The patient are instructed to abstain from oral intake for 6-8 hours to permit their stomach to empty
- Insensible losses continue during surgery
- Fluid shift to the third space(?) must be replaced
- Blood loss must be replaced either with crystalloid(3:1) or with colloid(1:1) or with blood component therapy (BCT)
- Compensatory stage hypovolumic patients develop severe hypotension during induction which is due to vasodilatation and hence vascular space must be filled.
- Urine output must be taken into account and that should be replaced.
What are the risks of inadequate fluid therapy?
- Post operative nausea and vomiting
- Pain
- Thirst, drowsiness
- Lactic acidosis
- Dehydration ketosis
- Acute renal failure
- Multi system organ failure
What are the risks of excessive fluid administration?
- Interstitial edema
- Impaired cellular metabolism
- Hemo dilution & Poor wound healing
- Decreased pulmonary compliance & pulmonary edema
- Heart failure
- Delayed return of bowel function
- Peri orbital edema and transient visual impairment
- Prolonged Hospital stay
How to assess patient’s volaemic (fluid) status?
- Basic tools like History taking
- Examination and interpretation of vital signs
- Fluid Intake& body fluids output chart
- Body weight
- Interpretation of laboratory investigations
What type of fluids to infuse?
The choice of intravenous fluids may broadly be categorized as colloids and crystalloids. Crystalloids are effective and appropriate for the initial management of extracellular compartment losses associated with hemorrhagic shock, major surgery or trauma.
Colloids are defined as having larger molecular weight and hence would remain in the vascular space for a longer period of time. colloid solutions are infused in an attempt to minimize interstitial edema within vital organs e.g. heart, lung and brain
Crystalloids:--
Most commonly administered crystalloid solutions are Normal saline and Ringer lactate. Administering large volume of 0.9% Normal saline can lead to increased NaCl level and produce metabolic acidosis.
Alternatively infusing large volume of RL can produce metabolic alkalosis as the lactate is metabolized to bicarbonate. Many patients present to the surgery with increased level of baseline potassium and increasing further could be hazardous. Presence of calcium in RL prohibits its use as carrier when administering citrated blood products. This calcium will cause RBC to aggregate.
Ringer acetate or plasmalyte solutions have composition similar to extra cellular fluid with respect to Sodium, Potassium, devoid of calcium and lactate and pH is 7.4
Though a theoretical advantage of infusing one litre of 5% dextrose in water provides 100gm of Glucose necessary for brain ,Glucose containing (hypo tonic) IV fluids are usually avoided because the increased glucose load can lead to several unwanted complications.
The advantages of crystalloids over colloids are that they are inexpensive and quickly effective at expanding intra vascular volume. But These solutions are reserved for surgeries lasting less than 4hours at the infusion rate of 4-6ml/kg/hr & did not cause significant interstitial edema. But in surgeries lasting more than 6hrs, the therapeutic window is narrowed and significant increase in interstitial fluid was reported.
Type of IV fluid |
Sodium (meq/l) |
Chloride (meq/l) |
Potassium (meq/l) |
Calcium (meq/l) |
Lactate (meq/l) |
PH |
Osmolarity (mOsm/kg) |
0.9%Normal Saline |
154 |
154 |
- |
- |
- |
5.6 |
308 |
Ringer lactate |
130 |
109 |
4.0 |
3.0 |
28 |
6.6 |
278 |
Plasma-Lyte |
140 |
98 |
5.0 |
- |
- |
7.4 |
290 |
5% dextrose |
- |
- |
- |
- |
- |
5.6 |
278 |
Extra cellular fluid |
140 |
108 |
4.5 |
2.0 |
5.0 |
7.3 |
290 |
Colloid solutions:--
They are more commonly used for fluid resuscitation in patients with severe fluid deficit. In case of massive haemorrage or burns victim, colloid may be infused while awaiting blood products for transfusion. They can also be used when there is need for large volume supplement & help to maintain plasma cncotic pressure Albumin is a naturally occurring plasma protein. Albumin provides approximately 70% of the plasma colloid oncotic pressure in normal human subjects. Human albumin is available for infusions as either 5% or 25% solution
Synthetic colloid solutions are Dextrans, Gelatins, Hydroxy ethyl starch.
HES –Hydroxy ethyl starch is available in several preparations and sub classified according to the molecular weight and presence of electrolytes. (FDA issued black box warning that HES not to be used in ICU)
Though colloid solutions are believed to remain in the intra vascular space for longer period ,their risks must be weighed against the benefits.
Comparison between colloids and crystalloids:--
Crystalloids |
colloids |
Distributed in extra cellular compartment |
Expands plasma volume |
80% leaves intra vascular compartment |
More expensive |
Large infusion causes dilutional coagulopathy & significant weight gain |
Infection & allergic response & larger volume ? coagulopathy |
Blood transfusions are rarely indicated in elective procedures. According to ASA guidelines blood should rarely be given if Hb is more than10 grams/dl and is mandatory if Hb is less than 6grams/dl. Blood transfusion must always be individualized and rate of loss, haemodynamic status and co morbid illness - all must be considered. Blood components are preferred after significant blood loss or where patient’s tissue oxygenation is compromised or hemostasis mechanism is affected
How much fluid we should administer?
Intra operative fluid Therapy is generally calculated by using Holiday and Segar formula (1957). It is generally agreed that the maintenance requirements for water of individuals is determined by their caloric expenditure.
For Water
- 4:2:1 rule- 4ml/kg/hr for first 10kg of body weight, 2ml/kg/hr for the second 10kg of body weight and 1ml/kg/hr for all tha additional Kg weight.
- 100:50:20 rule- 100ml/kg/day ( 100cal/kg/day for 0-10 kg)
50ml/kg/day (50cal/kg/day for 10-20kg)
20ml/kg/day (20cal/kg/day for all >20kg weight)
For Sodium= 1.0mEq/kg/d For potassium =0.75mEq/kg/d.
Traditional regimens for intra operative fluid administration:-
Standard fluid therapy:--
- Maintenance fluid as per 4-2-1 rule in adult
- Pre operative deficit correction- period of starvation in hours X maintenance fluid/hour
- Third space loss
For minor surgery-2-4ml/kg/hr
For major surgery- 6-8ml/kg/hr
- Blood replacement up to <10% blood volume loss - crystalloids3:1 or colloids 1:1
Avoid single unit blood transfusion instead BCT is better option
>10% blood volume loss – consider blood transfusion1:1
This calculated fluid should be infused in the first three hours as follows
First hour 1+half the2+3+4; second hour& third hour 1+ quarter of 2+3+4.
After third hour , fluid therapy is according to calculated maintenance , ongoing blood loss and
Third space loss
Expected Fluid loss during surgery &-additional requirement |
||
Degree of tissue exposure |
Type of surgery |
Addl. requirement |
Minor surgeries |
Hernia, hydrocele |
0-2-4ml/kg/hr |
Moderate surgery |
Breast surgery, cholecystectomy |
2-4-6ml/kg/hr |
Major surgeries |
Bowel resection, prostate surgery |
4-6-8 ml/kg/hr |
Restricted fluid therapy:--
In thoracic surgery fluid restriction is strongly advocated. Here the principle is that loss should be replaced but fluid overload in the form of weight gain should be avoided. Many randomized double blind studies published in this regard. Overall conclusion with those studies are restricted fluid regimen demonstrated a beneficial effect in pulmonary function and reduced incidence of post operative pulmonary complications but no much difference in length of hospital stay.
Goal directed fluid therapy:--
The concept is to restore the normal blood volume, cardiac output, there by maintaining circulatory function, the oxygenation, normal electrolyte acid base status and provide adequate nutrition. This is guided by invasive or sophisticated non invasive hemodynamic monitoring and usage of vasopressor or ionotropic drugs. If it is individualized depending on the objective feedback of Frank-Starling based fluid responsiveness, it is termed individualized goal directed fluid therapy.
But now we have the Doubt ‘Is it too much?’ WHY?
- In most of the situations, Patient’s pre operative hydration state is not correctly assessed
- For example, a 70 kg adult male having blood water of 42 litres(60% of lean body mass), Of this (2/3) 28L intra cellular, &(1/3)extra cellular volume is 14L ECV. This is further divided into plasma -3L and interstitial -11L. To maintain this, average fluid intake is two to three litres per day. Out of which, in a 6-8 hours of pre operative fasting for elective surgery , it is about 600 to 800ml only.
- But nowadays we advocate clear fluid/water intake up to 2hours pre operatively.
- In addition to this, hyper osmolarity and hypovolaemia activate ADH secretion and thereby enhancing renal water conservation.
- Hypovolemia activates rennin angiotensin mechanism , promoting sodium and water retention
- Bowel preparation, as a cause for dehydration is undertaken less frequently.
- Minimal invasive surgeries, Adequate Control of pain and administration of anti emetics have hastened the patient to return to pre operative status as earlier
- Temperature control, humidification systems, constant irrigation of peritoneum in open abdominal surgeries, endoscopic procedures whenever feasible,- further reduces insensible loss.
- The concept of a ‘third space’ was introduced in early 60s. Using some tracer techniques the extra cellular fluid volume was measured in patients undergoing major complicated abdominal surgeries for obstructive pathology. It was noticed that there was a decrease in the ECV which was not fully accounted by the measured blood loss. So It was hypothesized that fluid was sequestrated in areas known as third space- traumatized tissues, or GIT
- In the absence of major trauma or haemorrhage, large volume of fluid loading may lead on to hypervolaemia causing ANP release and damage to the endothelial glycocalyx.
Monitoring
Apart from clinical observation of pulse rate, volume, invasive or non invasive blood pressure, skin turger, pedal, peri orbital edema, cold extremities due to vasoconstriction following monitoring is essential to assess the fluid status/ condition
- by central venous cannulation & pulmonary artery catheterisation
- pulse pressure variation
- Esophageal Doppler monitoring- stroke distance estimation
- Trans Esophageal ECHO for real time direct visualization of stroke volume and cardiac motion
- pulse pleyth variability index using Massimo technology
- Lung USG- bed side evaluation to assess pulmonary congestion
- Arterial pulse contour analysis and Stroke volume measurement
What is the solution?
- Crystalloids in moderate volume should be used to replace insensible loss less than 0.5ml/kg/hr and urine output.
- Colloids are better choice for plasma deficit, acute blood loss and protein rich fluid
- Volume of colloid infusion should be around 1-2L
- Colloids should be better avoided in patients with liver or kidney diseases & also in chronic ICU patients
- There is no rationale for prescribing 1:3 ratio for blood: crystalloid infusion
- Overnight fasting does not deplete Intra vascular volume
- Third space does not exist
- Blood component therapy rather than whole blood transfusion is preferred unless there is acute haemorrhage and Hb <6-8 gm/dl
- Since life is a dynamic process, Algorithm are not to be fixed but rather should be dynamic and allow for individualized goal directed fluid therapy based on changing physiological status and response to the drug &fluid therapy.
- Fluid responsiveness is a qualitative assessment of patient’s ability to respond to fluid bolus & it should be assessed using dynamic indices such as Arterial pulse contour analysis and Stroke volume measurement or its surrogates in an uniform manner.
Are we ready for the change?
Inappropriate intravenous fluid therapy is a significant cause for patient morbidity and mortality and may result from either incorrect volume (too much or too little) or incorrect type of fluid.
Though insufficient fluid administration is readily identified by signs and symptoms of inadequate circulation and decreased organ perfusion , mild to moderate fluid overload has no precise symptoms but complications usually arise in pre existing cardio respiratory diseases and severe acute illness .
Administration of wrong type of fluid results in dearrangement of electrolyes, cellular volume and functions. So adequate and timely replacement of actual losses with appropriate preparations is mandatory.
In patients whose condition is uncomplicated, restrictive approach to peri operative fluid replacement with regular monitoring of electrolytes is better option.
No intra venous fluid infusion should be continued simply because it is routine.
References and for further reading:-
- Holt.k,SharrockNE-pathophysiology and clinical implications of peri operative fluid excess BrJ Anesthe2002;89(4).622-32
- Nisanevich.v,Felsenetein et al.Effect of intra operative fluid managementon outcome after intra abdominal surgery, Anesthesiology.2005;103:25-32
- Finfer.s, Bellomo.r et al.Acomparison of Albumin and saline for fluid resuscitation in intensive care unit. N.Eng.J Med;2004;350;2247-2256
- Yogendran.s, asokumar.B et al A prospective randomized double blind study of effect of intra venous fluid therapy on adverse outcomes on outpatient surgery. Anesth Analg.1995;80;682-686
- Sarah shabot, Donald prough 2011; fluid therapy Chapter 22, Section III; fluid therapy 202-209
- Doherty.M, Buggy.D.J intra operative fluid therapy: how much is too much? BJA advance accessJune1 ,2012
- C.L.Gurudatt peri operative fluid therapy: How much is not too much?;Ind.J.Anaesth.2012.jul-Aug:56(4):323-325
- Rob MacSweeney, Rachel Alexandra et al; Peri operative fluid therapy for adults;Ulster Med j 2013:82(3):171-178
- Lee.LA.Peri operative visual loss and anesthetic management.Curr Opin Anesthesiology 2013;26;375-381
- Elizabeth.A.M, Frost; perioperative fluids An evidence based review Anesthesiology News Special edition ;October 2014