Conference Lectures
Dr G.P.KIRUPAKARAN, MD;DA
SALEM, TAMIL NADU
POST OPERATIVE SHIVERING-CURRENT CONCEPTS
Shivering, an involuntary, oscillatory muscular activity, is a physiological response to core hypothermia in an attempt to raise the metabolic heat production .Post -operative shivering is one of the frequent, undesirable and unpleasant complications of both general and regional anaesthesia. IN homeo thermic species, a thermoregulatory system in hypothalamus coordinates defences against cold and heat to maintain internal body temperature within a narrow range, thus optimizing normal physiologic and metabolic function. Prolonged impairment of thermoregulatory autonomic control under anaesthesia along with the cold environment of operating rooms and cold infusion fluids, contributes to a fall in core body temperature, and hence shivering.
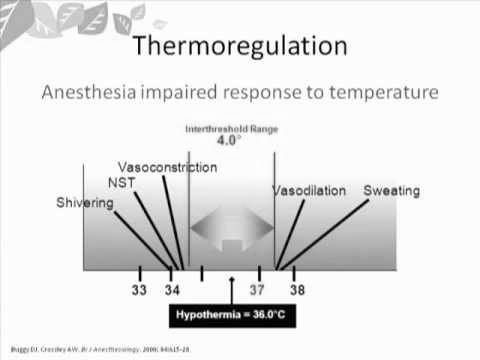
The normal human core temperature ranges from 36.5OC to 37.5OC. Thermal inputs are integrated at the level of the anterior hypothalamus, which compares peripheral information with a threshold value, or the set-point. Temperatures higher than this set point will trigger responses to cool the body, while temperatures lower than this set point will activate reflexes to warm the body. Both general and regional anaesthesia is known to affect the efficiency of this homeostatic system and may result in different degrees of post operative hypothermia. While general anaesthesia decreases the threshold by 2- 3oC, regional anaesthesia also decreases this threshold by 0.50C. In regional anaesthesia, vasoconstriction and shivering occurs above the level of block but in general anaesthesia muscle relaxants and other anaesthetic agents blocks these muscle contractions.
Other known causes of shivering include transfusion reactions, drug reactions, pre-existing high grade fever or bacteraemia, or infusion of contaminated intravenous fluids (fungal growth in dextrose containing fluids).In these situations the core temperature is either normal or elevated.
Perioperative hypothermia is the most common cause of shivering, though the exact
Incidence of each is difficult to evaluate, it may vary from 6 to 66%. Vigorous
Shivering increases metabolic heat production up to 600% above basal level .In a shivering patient, oxygen consumption may increase by 100% along with a linear increase in carbon dioxide production. Thus in a patient with limited myocardial oxygen reserve or known coronary disease, shivering may further compromise myocardial function. Shivering also increase intraocular and intracranial pressure, and may contribute to increased wound pain, delayed wound healing, and delayed discharge from postanesthetic care.
Shivering was observed to occur more frequently in the female gender and on use of thiopentone compared with propofol after general anaesthesia.
GRADING OF SHIVERING
Shivering is graded by using a scale similar to that validated by Tsai and Chu where:
0= No shivering.
1=Piloerection or peripheral vasoconstriction but no visible shivering.
2= Muscular activity in only one muscle group.
3= Muscular activity in more than one muscle group but not generalized.
4= Shivering all over the body.
MECHANISM
It is useful to consider thermoregulatory physiology in terms of a two-compartment model. A central core compartment, comprising the major trunk organs and the brain, accounts for two thirds of body heat content, maintained within a narrow temperature range (36.5–37.5°C) to facilitate cellular enzyme function. The peripheral compartment consists of skin and subcutaneous tissues over the body surface and the limbs. It represents about one-third of total body heat content. In contrast with the core, peripheral tissues undergo a wide variability of temperature, ranging from 2–3°C below to > 20°C below core temperature in extreme conditions. Maintaining core temperature within a narrow range requires the balancing of heat production and loss. This is achieved by a control system consisting of afferent thermal receptors, central integrating systems and efferent control mechanisms.
The mechanism which leads to shivering after anaesthesia is not very clear, but the probable mechanisms could be decrease in core body temperature secondary to sympathetic block; peripheral vasodilatation; increased cutaneous blood flow, which leads to increased heat loss through skin; cold temperature of operation theatre; rapid infusion of cold IV fluids; and effect of cold anaesthetic drugs upon the thermo sensitive receptors in the spinal cord.
Peri-operative heat loss occurs predominantly by radiation (60%), convection (25%), and evaporation of body fluids (10%). Radiation and convective heat loss depend on the difference between peripheral body temperature and ambient temperature. Convection also depends on the velocity of air movement around the body. Vasodilatation and sweating are the major autonomic mechanisms of increasing heat loss during anaesthesia. Sweating rates can reach > 1 litre h–1 for a short time, resulting in heat loss of up to 15 times BMR. In normal adults, the first response to a decrease in core temperature below the normal range (36.5–37.0°C) is Piloerection then followed by peripheral vasoconstriction. If core temperature continues to decrease, shivering commences. Normally, the threshold temperature for thermoregulatory vasoconstriction is 36.5°C and shivering commences at 36.0–36.2°C. General anaesthesia reduces these thresholds by 2-3OC
The principal autonomic mechanisms of preserving body heat and increasing heat production are vasoconstriction and shivering. The latter can increase heat production 6-fold. Non-shivering thermo genesis is particularly important in neonates and can increase heat production 3-fold. Cold stimuli induce nor epinephrine release in brown adipose tissue which uncouples oxidative phosphorylation. Therefore, the energy of glucose metabolism is released as heat, rather than stored as energy-releasing compounds, e.g. adenosine triphosphate (ATP). Exercise can increase heat production by as much as 20-fold at maximal intensity.
Effect of general and regional anaesthesia on thermoregulation
General anaesthesia reduces these thresholds by 2–3°C. General anaesthesia typically results in mild core hypothermia (1–3°C). This occurs in a characteristic 3-phase pattern.
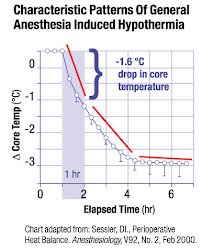
Phase 1 is a rapid reduction in core temperature of 1.0–1.5°C within the first 30–45 min. This is attributable to vasodilatation and other effects of general anaesthesia. Vasodilatation inhibits normal tonic vasoconstriction resulting in a core-to-peripheral temperature gradient and redistribution of body heat from core to peripheral tissues. General anaesthesia also reduces the threshold for activation of thermoregulatory vasoconstriction. Therefore, core temperature can become much colder before the re-set vasoconstrictor response can occur.
Phase 2 is a more gradual, linear reduction in core temperature of a further 1°C over the next 2–3 h of anaesthesia. This is due to heat loss by radiation, convection and evaporation exceeding heat gain which is determined by the metabolic rate. Radiation and convective heat losses in this phase are determined by the difference between peripheral and ambient temperature. Evaporation heat loss is exacerbated during major surgery where a greater surface area of tissue may be exposed to the environment.
Phase 3 is a ‘plateau’ phase where heat loss is matched by metabolic heat production. This occurs when anaesthetised patients become sufficiently hypothermic to reach the altered threshold for vasoconstriction which restricts the core-to peripheral heat gradient.
As with general anaesthesia, redistribution of body heat during spinal or epidural anaesthesia is the main cause of hypothermia. Because redistribution during spinal or epidural anaesthesia is usually confined to the lower half of the body, the initial
Core hypothermia is not as pronounced as in general anaesthesia (approximately 0.5°C). Otherwise, the pattern of hypothermia during spinal or epidural anaesthesia follows a similar pattern to that of general anaesthesia for the first two phases. The major difference in spinal or epidural anaesthesia is that the plateau phase does not emerge because vasoconstriction is blocked. Therefore, patients undergoing long procedures with combined general and epidural anaesthesia are at risk of a greater degree of hypothermia
Consequences of inadvertent hypothermia
The first clinical consequence of post anaesthetic shivering is discomfort to the patient. Another consequence is increased pain due to muscular contractions.
CARDIO VASCULAR
Unintended hypothermia can result in adverse consequences to the cardiovascular system. As mentioned previously, the body reacts to hypothermia by producing vasoconstriction. As a result, enhanced resistance leads to increased blood pressure and myocardial after load. This limits the ability of the myocardium to contract and prolongs signal conduction. A hypothermic patient may manifest with symptoms of tachycardia, hypertension followed by compensatory bradycardia. Ventricular fibrillation and arrhythmias can also occur with significant hypothermia. In addition, when core temperature falls by more than 1 degree C, the body activates the shivering mechanism and places large demands on the cardiovascular system. Upon emergence in the early postoperative period, adrenergic and metabolic responses can interfere with the balance between oxygen supply and demand, potentially leading to ischemia and myocardial infarction. Cardiac morbidity is the leading cause of death in the perioperative period. However, maintenance of normothermia throughout surgery has the potential of decreasing cardiac morbidity by 55%. A study by Frank et al showed a significantly greater incidence of postoperative hypoxemia, myocardial ischemia, and angina during the first 24 hours postoperatively in patients whose temperatures were less than 35 degrees C. The induced adrenergic response of the cardiovascular system to hypothermia is demonstrated by the cold pressor test, where a patient’s hand is immersed in an ice cold bath (4 degrees Celsius) for approximately 2 minutes. The heart rate and blood pressure immediately increase, resulting from enhanced levels of circulating catecholamines like nor epinephrine. Even mild hypothermia can trigger sympathetically mediated hypertension due to 100-700% increase of circulating nor epinephrine. In addition, cortisol increases have a significant role in the response to cold stress and are associated with immune inhibition.
COAGULATION
When the body’s core temperature is depressed, the patient develops coagulopathy and decreased platelet function. Blood loss is significantly increased with mild hypothermia, necessitating postoperative transfusions.
When undergoing surgical procedures, patients are at an even higher risk for blood clots due to hypothermia’s enhancing effects on blood viscosity and peripheral vasculature resistance. The body experiences diminished blood flow to the extremities, which can lead to blood stasis, decreased perfusion to the vital organs, and postoperative deep vein thrombosis and pulmonary emboli.
RENAL AND HEPATIC
Hypothermia has an effect on the kidneys as well, impairing the glomerular filtration rate and increasing blood urea nitrogen and creatinine levels.
Hepatic and pancreatic functions are also reduced, lessening the efficacy of drug metabolism. As a result, anaesthetic agents are metabolized more slowly, and the patient experiences longer emergence and enhanced recovery periods.
RESPIRATORY
The primary response of the respiratory system to hypothermia is hyperventilation that is followed by hypoventilation and abnormal breathing patterns. A decreased core body temperature leads to a leftward shift in the oxygen-haemoglobin dissociation curve, resulting in haemoglobin with a greater affinity for oxygen. The delivery of oxygen is therefore reduced, resulting in hypoxia, anaerobic metabolism, and lactic acidosis. The complications are worsened when the patient shivers due to the increased demand for oxygen and carbon dioxide production. Hypothermia also decreases bronchial arterial blood flow, which delays oxygen uptake and delivery to tissues. As oxygen exchange in the intrapulmonary system worsens, the body’s compensatory mechanisms become inadequate, and patient decline is inevitable.
HIGH RISK GROUPS
Throughout the patient population, many groups have a higher risk for developing hypothermia than others. For example, elderly patients have a significantly higher chance due to changes within the body as one ages. An elderly patient’s metabolic activity and capability to thermo regulate is depressed due to decreases in muscle mass and adipose tissue. In addition, the elderly have decreased circulatory function with increased vascular stiffness, which interferes with heat distribution and autonomic influences on vasculature. Conduction abnormalities, hypertension, and bradyarrhythmias are much more prevalent in the elderly. Anaesthesiologists must take these changes into consideration when caring for elderly patients undergoing surgery due to the increased risk of an adverse outcome. Infants, who have approximately three times the amount of body surface area to body mass ratio compared to adults, also have a high risk of developing hypothermia. Hypothermia is inversely related to amount of fat and the surface area to mass ratio. Infants are not able to utilize the shivering mechanism, and they are dependent on brown fat metabolism to normalize body temperature.
Lastly, patients who have certain medical conditions may be predisposed to developing hypothermia. Patients with hypothyroidism or cardiac pathologies, in addition to burn, cachectic, and trauma patients, are just to name a few. Patients placed on certain medications, like anti-hypertensives and anti-psychotics, can also experience an offset in the essential equilibrium between heat production and loss. Acknowledging the patient populations that have an increased risk for developing hypothermia is essential in striving to maintain an adequate body temperature perioperatively.
DRUG METABOLISM
Vasoconstriction also depresses hepatic blood flow, resulting in impaired drug metabolism and prolonged emergence from anaesthesia.
ANAESTHESIA TECHNICS
Both general and regional anaesthesia contribute to the development of hypothermia, so careful monitoring of temperature is required regardless of technique. All volatile anaesthetics impair thermoregulatory mechanisms. Commonly administered agents with vasodilatory properties are propofol, morphine, and meperidine. Opioids are known to increase the normal thermoregulatory threshold range from approximately 0.2 degrees C to as much as 4 degrees C, rendering the patient unable to adjust core temperature due to excessive vasodilatation. Due to the fact that in the elderly, diminished drug metabolism and anaesthetic-induced inhibition of the thermoregulatory response is more severe, use of the lowest possible effective dosage/concentration of anaesthetic agents is important.
SURGICAL WOUND INFECTIONS
There is evidence that wound healing is impaired and that patients are more susceptible to wound infection when hypothermia (<35ºC) occurs during surgery. Mild hypothermia (34.7ºC) increased the incidence of wound infection threefold (19% versus 6%) compared with normothermic patients (36.6ºC).The incidence of surgical wound infection is directly related to subcutaneous wound tissue oxygen tension. In turn, this is compromised by hypothermia-induced vasoconstriction. Moreover, mild hypothermia directly impairs neutrophil function.
Prevention and treatment of perioperative hypothermia
There are three basic strategies for the prevention and treatment of peri-operative hypothermia:
(i) Minimising redistribution of heat;
(ii) Cutaneous warming during anaesthesia; and
(iii) internal warming.
Minimising redistribution of heat
This may be achieved by:
(i) Pre-operative warming of peripheral tissue; and
(ii) Pre-operative pharmacological vasodilatation.
Pre-operative warming of peripheral tissue
This reduces the normal core-to-peripheral temperature gradient so that induction of anaesthesia does not result in the sudden core hypothermia seen in Phase 1. However, to be effective, this would require subjecting patients to over 1 h of exposure to a source of radiated heat pre-operatively which may not be practicable.
Pre-operative pharmacological vasodilatation
This facilitates core-to-peripheral redistribution of heat before anaesthesia; it does not compromise core temperature because patients are not anaesthetised and their thermoregulatory responses are intact. Oral nifedipine, taken pre-operatively, has
been shown to reduce effectively the extent of the initial redistribution hypothermia by 50%.
Cutaneous warming during anaesthesia
Passive insulation
A single layer of any insulator (e.g. space blanket) reduces cutaneous heat loss by approximately 30% because it traps a layer of still air between it and the skin. Adding further layers of passive insulation does little or nothing to preserve core temperature.
Active warming
Active warming systems maintain normo thermia much more effectively than passive insulation. The electrically powered air heater-fan and patient cover is effective because it replaces cool room air with warmed air and also because convection
increases heat gain when the forced air is warmer than skin.
Active warming by circulating water mattresses is relatively ineffective because heat is applied only to the patient’s back where relatively little heat is lost. They have been superseded by forced air warming devices.
Internal warming
Fluid warming
Fluids should be warmed to body temperature prior to infusion. The administration of one litre of fluid at room temperature decreases core temperature by 0.25°C. Fluid warming devices should be used when large amounts of fluid or blood replacement are anticipated. Fluid warming alone will not prevent core hypothermia.
Airway humidification
This contributes little to preservation of core temperature because < 10% of metabolic heat loss occurs via the respiratory tract.
Invasive internal warming techniques
Cardiopulmonary bypass transfers heat at a rate and magnitude not seen in any other situation. Peritoneal dialysis is also very effective but neither technique is relevant to regular practice.
Amino acid infusion
Amino acid infusion during anaesthesia increases metabolic rate and patients are less hypothermic compared with those given the same volume of crystalloid. This technique has not gained wide-spread acceptance because of doubts about the effect on cardiac outcome of increased metabolic rate during anaesthesia.
PHARMACOLOGICAL INTERVENTIONS
Pharmacological intervention does not raise body temperature, but resets the shivering threshold to a lower level, thereby decreasing rigors and its episodes. The neurotransmitter pathways involved in shivering are complex and involve opioids, Alpha-2 adrenergic, serotenergic, and anticholinergic receptors. By virtue of this fact, drugs acting on these systems are utilized in treatment of this condition, the perioperative Meperidine is more effective in the treatment of patient shivering than other opioid agonists or agonist–antagonists. Tramadol, clonidine, butarphanol, nalbupine, ondansetron and ketamine in low doses are used with varying amount of success.
Conclusions
Peri-operative hypothermia is associated with cardiac morbidity, increased blood loss, surgical wound infection and increased duration of hospitalisation. Most surgical patients are at risk of the many adverse outcomes of mild hypothermia,
particularly elderly, high-risk patients undergoing major surgery. The particular method of maintaining core temperature above 36.5°C is unimportant but use of forced-air convective warmers probably represent the most efficient, practical strategy of preventing core hypothermia and restoring normal core temperature in current practice.