| |
Scenario in 2009 |
| |
Cuffed vs non-cuffed endotracheal tubes for pediatric anesthesia |
| |
 |
Pro-Con Debate
TONI WEBER/ NADE` GE SALVI/GILLES ORLIAGUET
Pediatric Anesthesia 2009 19 (Suppl. 1): 46–54 | |
| |
 |
| |
Introduction |
| |
In choosing the tube size, one must consider choosing between cuffed and uncuffed tubes. For many years, uncuffed tubes have been recommended for children under 8 yrs of age (the pediatric larynx goes through a transformation from cone-shaped to cylindrical at 8 yr of age). The uncuffed tube is to be positioned to form a seal at the cricoid ring; the narrowest portion of the child’s airway. However, a great debate has developed in the world of anesthesia when choosing between a cuffed tube and uncuffed tube.
|
| |
Here is an interesting Pro-Con debate of cuffed vs non cuffed tubes for pediatric anesthesia published in Pediatric Anesthesia 2009.
|
| |
Uncuffed tubes should continue to be used in pediatric anesthesia
Toni Weber |
| |
The development of the cuffed pediatric endotracheal tube into pediatric practice, has added Key concerns include:
|
| |
 The need to use a smaller internal diameter (ID) tube in order to place the cuff, The need to use a smaller internal diameter (ID) tube in order to place the cuff, |
| |
 The need for additional monitoring and adjusting of cuff pressure The need for additional monitoring and adjusting of cuff pressure |
| |
 The potential morbidity from the cuff by pressure, The potential morbidity from the cuff by pressure, |
| |
 The potential for inappropriate tube placement or cuff herniation. The potential for inappropriate tube placement or cuff herniation. |
| |
Points against cuffed ETT (CTT) |
| |
 Intubation with an ETT (whether cuffed or uncuffed) that is too large can lead to laryngeal damage, tracheal damage and subglottic stenosis with significant long-term morbidity which in the most extreme cases may require tracheostomy and laryngeal or tracheal reconstruction. Intubation with an ETT (whether cuffed or uncuffed) that is too large can lead to laryngeal damage, tracheal damage and subglottic stenosis with significant long-term morbidity which in the most extreme cases may require tracheostomy and laryngeal or tracheal reconstruction. |
|
| |
 One of the obviously avoidable factors for excessive mucosal pressure is either from an over-large uncuffed endotracheal tube (UTT) or an inflated cuff in a cuffed endotracheal tube (CTT). One of the obviously avoidable factors for excessive mucosal pressure is either from an over-large uncuffed endotracheal tube (UTT) or an inflated cuff in a cuffed endotracheal tube (CTT). |
|
| |
 The overall incidence of intubation trauma in the pediatrics is significant with the vast majority of problems (82%) being ascribed, based on endoscopic examination, to an excessively large ETT rather than the intubation procedure itself. The overall incidence of intubation trauma in the pediatrics is significant with the vast majority of problems (82%) being ascribed, based on endoscopic examination, to an excessively large ETT rather than the intubation procedure itself. |
|
| |
 The adoption of a CTT does not protect the patient from airway trauma. The adoption of a CTT does not protect the patient from airway trauma. |
|
| |
 Over a 10 year period (1987–1997) Holzki reported four severe laryngeal injuries caused by CTT. Four years later the same author reported six similar lesions in 1 year. Over a 10 year period (1987–1997) Holzki reported four severe laryngeal injuries caused by CTT. Four years later the same author reported six similar lesions in 1 year. |
|
| |
 Concerns have also been raised about the potential for tube misplacement. The distance from glottis to carina is relatively short and the design of some cuffed tubes has been such that when the cuff is correctly placed just below the vocal cords, the tip of the tube is already at the carina. Concerns have also been raised about the potential for tube misplacement. The distance from glottis to carina is relatively short and the design of some cuffed tubes has been such that when the cuff is correctly placed just below the vocal cords, the tip of the tube is already at the carina. |
|
| |
 The cuffed tube selected for intubation will be smaller than the uncuffed tube because cuffed tubes are manufactured with thicker walls and the cuff ‘adds’ the additional diameter to form the seal with the trachea. As a result choosing a cuffed tube necessitates using a tube with a smaller ID. The difference of a 3.0 mm tube compared to a 4 mm tube represents a three-fold increase in airway resistance leading to potential problems increased work of breathing and the problems with retention of secretions and even airway occlusion. The cuffed tube selected for intubation will be smaller than the uncuffed tube because cuffed tubes are manufactured with thicker walls and the cuff ‘adds’ the additional diameter to form the seal with the trachea. As a result choosing a cuffed tube necessitates using a tube with a smaller ID. The difference of a 3.0 mm tube compared to a 4 mm tube represents a three-fold increase in airway resistance leading to potential problems increased work of breathing and the problems with retention of secretions and even airway occlusion. |
|
| |
 In the long history of the UTT the potential disadvantages of undersized tubes have been well documented. These include variable air leak, difficulties in effectively ventilating the patient with lung disease or allowing atelectasia, environmental contamination of anesthetic gasses, risk of aspiration, and difficulty in accurate measurement of end tidal CO2 concentration. In the long history of the UTT the potential disadvantages of undersized tubes have been well documented. These include variable air leak, difficulties in effectively ventilating the patient with lung disease or allowing atelectasia, environmental contamination of anesthetic gasses, risk of aspiration, and difficulty in accurate measurement of end tidal CO2 concentration. |
|
| |
 While tight fitting tubes confer benefit in patients with critical ventilation (such as pulmonary hypertension) the safe pressure in the child with cardiac compromise remains unknown. While tight fitting tubes confer benefit in patients with critical ventilation (such as pulmonary hypertension) the safe pressure in the child with cardiac compromise remains unknown. |
|
| |
 The sheer numbers of manufacturers making cuffs, the types of design of cuff (high-volume low pressure vs standard design), and the lack of standardization of the tube design have been very confusing. The sheer numbers of manufacturers making cuffs, the types of design of cuff (high-volume low pressure vs standard design), and the lack of standardization of the tube design have been very confusing. |
|
| |
 A majority of pediatric anesthetists interviewed in a recent UK survey felt that minimal benefit could be gained from cuffed tubes. More interestingly, all of the responding anesthetists and 45% of the intensivists reported that they did not routinely monitor the intracuff pressure, when using a cuffed tube. A majority of pediatric anesthetists interviewed in a recent UK survey felt that minimal benefit could be gained from cuffed tubes. More interestingly, all of the responding anesthetists and 45% of the intensivists reported that they did not routinely monitor the intracuff pressure, when using a cuffed tube. |
|
| |
 Cuff pressures do not remain static due to temperature effects, gas exchange and local factors including cuff movement, muscle relaxation, and anesthetic depth. Increasing cuff pressure promotes mucosal damage while reduced pressure can allow leak. Cuff pressures do not remain static due to temperature effects, gas exchange and local factors including cuff movement, muscle relaxation, and anesthetic depth. Increasing cuff pressure promotes mucosal damage while reduced pressure can allow leak. |
|
| |
 Modern cuff design may reduce complications but meticulous pressure monitoring is mandatory which is feasible in intensive care there might be clear benefit, but in a rapid turnover operating list with healthy patients this might not be a feasible or sensible option. Modern cuff design may reduce complications but meticulous pressure monitoring is mandatory which is feasible in intensive care there might be clear benefit, but in a rapid turnover operating list with healthy patients this might not be a feasible or sensible option.
|
|
| |
In conclusion, despite potential advantages of the CTT they are yet to prove themselves against a technique that has a safety and reliability record over 40 years.
|
| |
CTT also have disadvantages, with a smaller margin of safety and a requirement for precise positioning. Undoubtedly they have a place in pediatric anesthesia but with their increased cost, added complexity and the continuing problems associated with applying cuffed tubes in the youngest infants, they remains a selective tool for the older child.
|
| |
Cuffed tracheal tubes in routine pediatric anesthesia
Nade`ge Salvi M.D., Gilles Orliaguet MD. Ph.D. |
| |
Three major arguments were cited in favor UTT as of choice in paediatric anaesthesia.
|
| |
 |
Firstly, the use of a UTT was supposed to reduce the risk of laryngeal mucosa injury and thus the risk of secondary subglottic stenosis. |
| |
 |
Secondly, the use of a cuffed tracheal tube (CTT) was not required because of anatomic considerations, such as a narrow subglottic region of the trachea. |
| |
 |
Thirdly, the choice of a CTT requires the use of a tube with a smaller internal diameter, leading to higher respiratory airway pressures, as well as an increased work of breathing and risk of tube obstruction. |
| |
But these latter arguments were only relevant when children breathed spontaneously during anesthesia with ether or in the neonatal intensive care unit.
|
| |
The use of an adapted size of CET is not associated with an increased risk of respiratory complications.
|
| |
Recent studies have shown that the use of CTT was safe in pediatric anesthesia as well as in PICU |
| |
| Khine et al. in 1997: | Compared the use of CTT and UTT in pediatric anesthesia.They found no more croup in the CTT group as compared with the UTT group during the postoperative period. |
| James in 2001: | ‘The little evidence we have is that cuffed tubes are not more dangerous than uncuffed tubes’. James noted that a reduction of air leak as an important quality ascribed to cuffed endotracheal tubes. A sealed system allows for consistency in administration of tidal volumes and positive end expiratory pressure as well as provides for better measurement of lung compliance and airway resistance. |
| Murat in 2001: | She showed that respiratory complications in the recovery room were not associated to the use of CTT. CTT in routine practice reduces sevoflurane and N2O concentrations measured on anesthesiologists in the operating room, from 48.1 ppm and 192 ppm to 0.3 ppm and 29.4 ppm, respectively. |
| Duracher et al. in 2008: | Evaluated the use of CTT as the croup in predicting the correct size of CTT in pediatric anesthesia. Their secondary outcome was the incidence of post intubation respiratory complications.They reported six cases of complications (2.9%). In three cases due to the use of CTT of an incorrect predicted size. No tracheal reintubation or subglottic stenoses were recorded and there were no long-term complication. |
| Newth et al. in 2004: | Evaluated the safety of CTT in critically ill children hospitalized in a PICU. The primary outcome was the frequency of post extubation croup following long-term tracheal intubation using either a CTT or UTT. They found no difference between the two groups. |
| Meyer et al. in 2000: | Demonstrated that the occurrence of laryngotracheal complications after emergency tracheal intubation in severely injured children was not related to the use of a CTT. |
| Eschertzhuber et al in 2010: | Noted that cuffed tubes reduce the amount of leaked anesthetic gases in the operating room. This gas leak has both environmental pollution implications as well as financial implications as anesthetics are being wasted. |
| Gopalareddy et al in 2007: | Demonstrated a reduction in tracheal aspirates containing gastric pepsin found in patients with cuffed tubes (53%) vs uncuffed (100%). | |
| |
Points in favour of cuffed ETT (CTT) |
| |
 |
The main factor constantly found for laryngotracheal injury is the use of an oversized tracheal tube. |
|
| |
 |
No study has demonstrated an increased risk of airway complications related to the use of CTT provided a CTT of appropriate size is chosen and the cuff pressure is monitored and adapted. |
|
| |
 |
Tracheal intubation with a CTT is probably the most reliable mean to ensure adequate positive pressure ventilation. In contrast air leak during mechanical ventilation with a UTT may compromise tidal volume or airway pressures and lead to hypoxemia, altered pulmonary artery pressure, excessive variability of PaCO2 etc. |
|
| |
 |
The use of CTT allows positive end-expiratory pressure (PEEP) to be used reliably. |
|
| |
 |
Reduced gas leak also allows techniques such as low fresh gas flow anesthesia in a circle system to be used, with accurate monitoring of inspired and expired gas composition. |
|
| |
 |
Reducing air leak, particularly if this allows a low flow circle system reduces consumption of volatile agents reduces atmospheric pollution and can lower the cost of anesthesia. |
|
| |
 |
CTT is the decrease in the risk of gastric content aspiration. |
|
| |
 |
If a CTT is used an appropriately sized tube must be selected of adequate internal diameter (ID). |
|
| |
 |
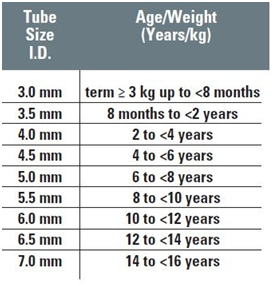
Khine’s Formula : Cuffed tube size (mm ID) = (age ⁄ 4) + 3 (Khine’s formula underestimated the size of CTT by 0.5 mm) Duracher et al. Formula: Children 1 year of age: cuffed tube size (mm ID) = (age ⁄ 4) + 3.5 |
|
| |
 |
Another very important factor to take into account to prevent postintubation laryngeal injury is the outer diameter (OD) of the tube. So, the choice of an optimal size fitted CTT requires to take into account not only the ID but also the OD. |
|
| |
 |
Another challenge seems to be the adequate placement of the cuff relative to the cricoid ring. |
|
| |
 |
“Ideally cuffed paediatric tracheal tube should have a high-volume-low pressure cuff with a short cuff length, adequate depth markings and not allow the cuff to be inflated in the subglottic region” |
|
| |
 |
During anaesthesia using a N2O⁄ oxygen gas mixture the Pcuff increases because of N2O diffusion into the cuff. This problem mainly occurs during the first 105 min and may potentially lead to tracheal damages because of a decrease in the tracheal perfusion pressure. |
|
| |
 |
Several studies have described different ways of filling the cuff in order to prevent both initial as well as secondary cuff over inflation during N2O anesthesia. |
|
| |
 fill the cuff with an N2O-oxygen gas mixture
fill the cuff with an N2O-oxygen gas mixture |
|
| |
 the cuff filled with normal saline (NOT RECOMMENDED) the cuff filled with normal saline (NOT RECOMMENDED) |
|
| |
 |
But safe attitude during N2O anesthesia is certainly to monitor the Pcuff continuously and to remove iteratively the gas in excess from cuff to maintain Pcuff around 20 cmH2O. |
|
| |
In conclusion, The increased cost of CTT compared to UTT is greatly compensated by the decrease in the reintubation rate, reducing the cost of using different tracheal tubes (at least two), as well as by the reduction in halogenated agents consumption permitted by fresh gas flow anaesthesia.
|
| |
CET can be used routinely in pediatric anesthesia, intensive or emergency care provided a tube with an adequate high-volume low-pressure cuff is selected and some important precautions are carefully respected including appropriate choice of a CET size, careful Pcuff monitoring throughout the case and adjustment of this pressure as necessary.
|
| |
| Conclusions: The routine use of uncuffed tubes in both pediatric anesthesia and intensive care has been demonstrated to have an excellent safety record over many years. It is therefore essential that progressing to the more expensive cuffed tube, which requires cuff monitoring and meticulous tube placement, is truly progress. There is also no clear view or data to inform the practitioner as to what age or size of tube is the lower limit for cuffed tube and this clearly requires further work. | |
| |
Source: Cuffed vs non-cuffed endotracheal tubes for pediatric anesthesia; Pediatric Anesthesia Volume 19, Issue Supplement s1, pages 46–54, July 2009
|
| |
Scenario in 2013 |
| |
Cuffed versus Uncuffed Endotracheal Tubes inPediatric Anesthesia |
| |
The Debate Should Finally End
Anesthesiology 2013 |
| |
 |
| |
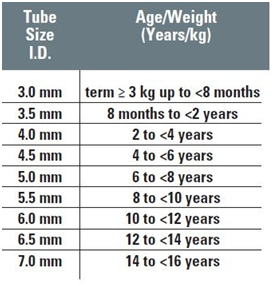
Microcuff® (Kimberly-Clark, Roswell, GA), which has been specifically designed for use in pediatric anesthesia. Two important modifications are:
|
| |
 |
First, the cuff is made of ultrathin (10 microns) polyurethane, which allows a more effective tracheal seal at pressures below those known to cause tracheal mucosa pressure necrosis. |
| |
 |
Second, the cuff is physically located more distally on the endotracheal tube shaft, facilitated by the omission of the Murphy eye. This feature more reliably places the cuff below the nondistensible cricoid ring and theoretically reduces the chance of an accidental main bronchus intubation. |
| |
Recommended Pediatric Microcuff Tube Size Selection |
| |
 |
| |
Uncuffed endotracheal tubes were preferred because the absence of a cuff allowed for a relatively larger internal diameter endotracheal tube. This allowed easier suctioning of secretions and a lower resistance to spontaneous ventilation.
|
| |
For the children of any age who undergo general anesthesia for medical or surgical procedures, the use of an uncuffed tube is generally safe, and associated with a low incidence of postextubation stridor, but there are drawbacks to having a ventilation leak around the tube.
|
| |
These include
|
| |
 |
An inaccurate capnographic tracing |
| |
 |
Inaccurate spirometric tidal volume measurement, |
| |
 |
Inaccurate end-tidal anesthetic level measurement |
| |
 |
Waste and increased cost of inhaled anesthetics |
| |
 |
Increased pollution of the operating room environment |
| |
 |
Increased airway fire risk |
| |
 |
Possible need to change the endotracheal tube to a different size (often only recognized after the surgical procedure has begun), |
| |
 |
Lack of ability to regulate the tracheal seal with change in respiratory system compliance, and |
| |
 |
An increased risk of microaspiration.
|
| |
Claims that cuffed endotracheal tubes predispose to glottic injury or an increased chance of bronchial intubation have not been substantiated clinically.
|
| |
Studies of freshly extubated neonatal larynges demonstrate damage to all areas of the glottic and subglottic regions. The rigid cricoid ring and the vocal folds are particularly susceptible to damage from mucosal shear because of the lack of any substantial submucosal layer in these areas.
|
| |
This is most likely what happens when an uncuffed endotracheal tube is used, which has a large enough external diameter to provide adequate ventilation without an excessive leak, especially with movement of the infants’ head and neck.
|
| |
Nevertheless, all children requiring tracheal intubation should benefit from a standard type of endotracheal tube that is associated with the best evidenced-based outcomes. This endotracheal tube should contain a high-volume, low-pressure cuff, with a standard ratio of internal to external diameter, and clear length markers along the tube.
|
| |
| Except for unique clinical circumstances (e.g., purposeful bronchial intubation for neonatal thoracic surgery and lung isolation), there is no longer a feasible role for the use of the uncuffed tube in pediatric anesthesia, or in chronically ventilated children beyond the neonatal period. | |
| |
Source: Cuffed versus Uncuffed Endotracheal Tubes in Pediatric Anesthesia: The Debate Should Finally End; Anesthesiology: March 2013 - Volume 118 - Issue 3 - p 500–501
|
| |
Ref: KIMBERLY-CLARK MICROCUFF Pediatric Endotracheal Tube – Brochure
|