| |
How to set your room
|
| |
The Practical guide for the everyday practices |
| |
Ahmad Mustapha Abou Leila |
| |
The Must-Dos |
| |
Check your Anesthesia Machine |
| |
 |
Turn on |
 |
O2-Air-N2O attached(look at the pipes, the pressure monitor) |
 |
Turn On the Ventilator
|
 |
Check for circuit leak
|
 |
Check the Soda Lime(purple or grey)
|
 |
The Scavenger is Open-the risk of pollution |
 |
The Vaporizer –The level of gas |
|
| |
Always Prepare set for general anesthesia |
| |
You will need them |
| |
 |
For the regular induction |
 |
For emergent intubation |
 |
For sedation |
 |
For regional anesthesia conversion into general anesthesia |
|
| |
| Always Prepare Vasopressor set |
 |
 |
Phenylephrine (0.1mg/ml) -Hypotension+ Tachycardia |
 |
Ephedrine (6mg/ml) -Hypotension+ Bradycardia |
 |
Atropine (0.1mg/ml) -symptomatic bradycardia |
| |
|
| |
Check for the SALT |
| |
 |
S: Suction |
 |
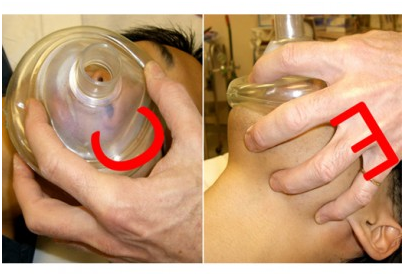
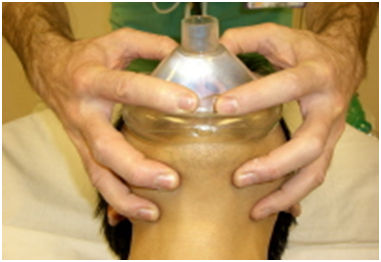
A : Ambu Bag-Airway |
 |
L:Laryngoscope |
 |
T:Tubes |
|
| |
Check the monitors Preoperatively:
|
| |
 |
Read the chart thoroughly
|
 |
The patient Name
|
 |
The peroperative Drugs
|
 |
The planned surgery
|
 |
The consultations
|
 |
The anesthesia Preoperative notes
|
|
| |
Quick re-assessment:
|
| |
 |
Air way |
 |
NPO hours |
 |
Anticoagulation |
 |
Allergies |
|
| |
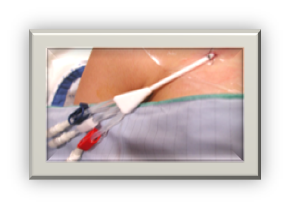
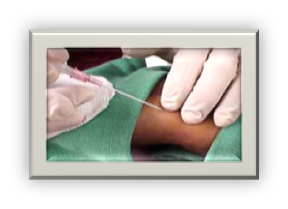
IV SITE :
|
| |
 |
Check for previous mastectomy, axillary dissection ,AV fistula, site of surgery before IV prick |
 |
Otherwise choose the left hand (most patient are right handed and it is easier for us) |
 |
Avoid the positional IV (near joints ) |
|
| |
The Gauge:
|
| |
 |
Small gauge (paedatrics, HF, Renal failure ,local case)
|
 |
Big gauge (work near big vessels, Trauma, spinal, Burn) |
|
| |
The solution:
|
| |
 |
LR most cases |
 |
NSS for (renal failure, Neuro cases) |
 |
Dextrose containing fluid in neonatal surgeries |
 |
Voluven for spinal cases, burn, risk of bleeding |
 |
Blood (call for blood units if risk of bleeding, preop anemia) |
 |
FFP (patient on warfarin, massive transfusion) |
 |
Platelets (platelets dysfunction) |
|
| |
 |
| |
Give some sedation before you go into the room….the patent in extreme anxiety |
| |
In Theatre:
|
| |
 |
| |
| Check the OR table ….not working |
 |
| Call the Orderly….fix it before u induce GA |
 |
Machine checked |
 |
SALT checked |
 |
Chart checked |
 |
IV secured |
 |
Vitals checked
|
 |
Table checked |
|
|
| |
| |
| |
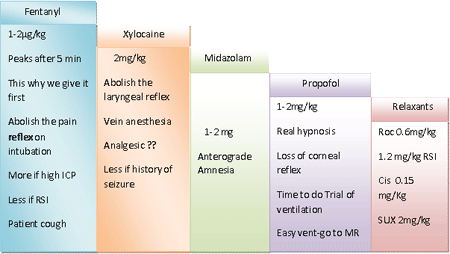
Induction:
|
| |
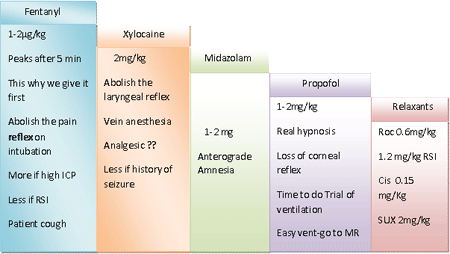
The sequence of regular induction |
| |
 |
| |
Special scenarios:
|
| |
 |
Pediatrics …higher Propofol |
 |
Elderly …lower Propofol |
 |
Shock…ketamine,etomidate
|
 |
Mediastinal mass…sevoflurane induction |
 |
Neuro…thiopentone
|
 |
High ICP... add β-blockers
|
 |
RSI…Propofol and SUX only |
|
| |
Tube selection and insertion: |
| |
| Patient related: |
 |
 |
female tube 7-7.5 |
 |
Male tube 8-8.5 |
 |
pediatrics age/4+4 |
|
| Surgery related |
 |
ENT:preformed tube |
 |
SML:MLT tube |
 |
Thyroid: Reinforced tube |
 |
Thoracic: DLT |
|
| Uncuffed till age of 8….. Contraversial? |
| Depth of insertion |
 |
Adult :height/10 + 5 |
 |
Peds :age in years + 10 |
|
| Nasal intubation - Smaller size tube |
| Depth of insertion: Oral depth + 3 |
| |
|
| |
Now you can put your invasive monitors if needed: |
| |
|
| |
Monitoring: |
| |
 Pulse Oximetry/ ECG/Temp Pulse Oximetry/ ECG/Temp |
| |
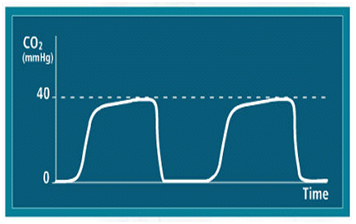
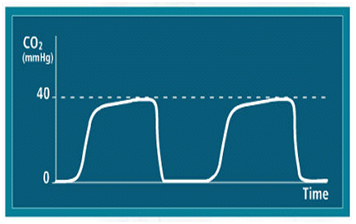
 Capnography Capnography |
| |
 Invasive/Non invasive BP Invasive/Non invasive BP |
| |
 CVP/ CWP CVP/ CWP |
| |
 |
CVP 0-5mmHg Liver Resection |
 |
CVP 5-9mmHg Semi sitting Craniotomy |
 |
CVP 8-12mmHg Septic patient |
 |
CVP>15mmHg Fontane patient |
|
| |
 Urine Output Urine Output |
| |
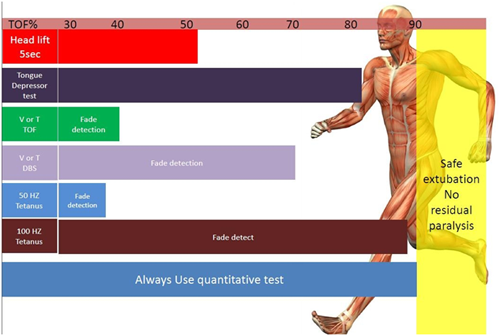
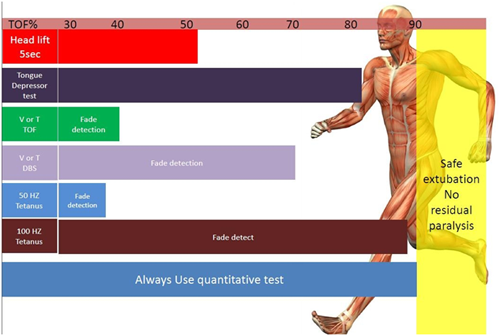
 Nerve Stimulator Nerve Stimulator |
| |
 |
TOF=0 in Neuro,Eye |
 |
TOF =1 in other cases |
 |
Deep parlysis needed PTC 0 |
 |
Face more resistant than thumb |
 |
(twitch in the face doesn’t mean twitch in the thumb) |
|
| |
 Lab: Lab: |
| |
| |
Baseline ABGS |
 |
Assess PaCo2-ETCO2 gradient |
 |
Oxygenation PaO2/fiO2..>200 it is OK |
 |
Hct |
 |
Electrolytes |
|
| |
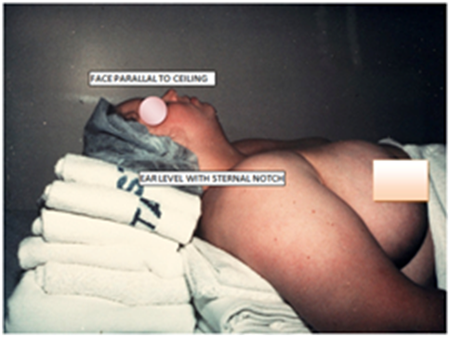
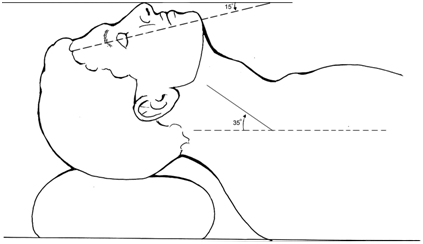
Patient Positioning: |
| |
 |
Watch for Nerve injury |
 |
Watch for Haemodynamic changes |
 |
Watch for ETT position
|
|
| |
Remember |
| |
 |
| |
Maintenance phase: |
| |
 |
| |
Avoid Hypothermia: |
| |
 |
Increase solubility of inhalation agents |
 |
Decrease metabolism |
 |
Increase risk of bleeding |
 |
Increase risk of wound infection |
 |
Acidosis |
 |
Post operative shivering |
 |
Arrhythmias |
|
| |
Watch for the blood loss: |
| |
 |
| |
Allowable Blood Loss (ABL): |
| |
|
| |
Hi = initial Hct |
| |
Hf = final lowest acceptable Hct |
| |
Estimated Blood Volume (EBV): |
| |
| EBV = weight (kg) x average blood volume |
|
| |
| Average blood volumes |
| Age |
Blood volume |
| Premature Neonates |
95 mL/kg |
| Full Term Neonates |
85 mL/kg |
| Infants |
80 mL/kg |
| Adult Men |
75 mL/kg |
| Adult Women |
65 mL/kg |
|
| |
Normal Hct Values |
| |
|
| |
Example: |
| |
Question: Before surgery is to take place, what is the estimated blood volume (EBV) of a female patient weighing 50 kg? Also, what is the allowable blood loss (ABL) of this patient if her Hct is 45? |
| |
In the example above, EBV = 50kg x 65 (adult woman's blood volume) = 3250 |
| |
The initial Hct (Hi) = 45%, her current Hct |
| |
The final lowest acceptable Hct (Hf) = 30% (What ever cut off is used clinically to decide how low the individual's Hct will be allowed to drop. Thirty percent is used in this calculator but in reality this will vary from case to case.) |
| |
So the example would look like this: |
| |
Using this rough estimate, the patient in this example could lose 1083 mL of blood without needing a transfusion. |
| |
Estimating blood loss: |
| |
 |
Dry sponges |
 |
4x4 hold ~ 10 mL blood |
 |
Ray-techs ~ 10-20 mL blood |
 |
Lap sponges ~ 100 mL blood |
|
| |
Pediatric cases should have sponges & gauze weighed for blood loss( 1GM = 1ML of blood) |
| |
Blood loss replacement: |
| |
Replace 1 mL blood with: |
| |
 |
3 mL crystalloid (i.e. NS, Dextrose, LR) |
 |
1 mL colloid (i.e. albumin, Dextran) |
 |
1 mL whole blood |
 |
1 mL PRBC |
|
| |
Blood Transfusion: |
| |
| Hb level |
Recommendation |
| > 10 |
inappropriate |
| 7-10 |
Likely to be appropriate if signs of impaired O2 Delivery |
| < 7 |
appropriate |
| < 6 |
Highly recommended |
|
| |
Watch out: |
| |
| BP |
HR |
Explanation |
 |
 |
High sympathetic state: Pain, awarness, adrenaline injection Pheo, thyroid storm |
 |
 |
Hypovolemic, septic patient, carcinoid crisis, anaphylaxis |
 |
 |
High fentanyl dose, Neostigmine, B-blockers, spinal shock |
 |
 |
After phenylephrine , Cushing reflex |
|
| |
Tests to assess recovery: Tests to assess Depth |
| |
 |
| |
Ahmad M. Abou Leila |